Sjogren’s syndrome (SS) is a chronic autoimmune disease primarily characterized by the body’s immune system mistakenly attacking its moisture-producing glands, particularly the salivary and lacrimal (tear) glands. This leads to symptoms such as dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca). However, Sjogren’s syndrome is much more complex than its hallmark symptoms suggest, affecting various organs and body systems in some patients, thereby earning its place as a systemic autoimmune disorder.
Table of Contents
ToggleOverview of Autoimmune Disorders
Before delving deeply into Sjogren’s syndrome, it’s crucial to understand what an autoimmune disorder is. In autoimmune diseases, the immune system, which normally protects the body against harmful invaders like bacteria and viruses, begins to attack healthy tissues. In Sjogren’s syndrome, this results in inflammation and damage to the moisture-secreting glands, though other organs can be affected as well. Autoimmune diseases, including Sjogren’s, vary widely in their severity and presentation, making diagnosis and treatment a nuanced process.
Historical Background
Sjogren’s syndrome is named after the Swedish ophthalmologist Henrik Sjögren, who first described the condition in 1933. While his early work focused on the symptoms of dry eyes and mouth, subsequent research revealed that the syndrome could affect the entire body, leading to systemic complications. Over the decades, understanding of Sjogren’s syndrome has grown, yet its exact cause remains elusive, contributing to ongoing challenges in diagnosis and treatment.
Types of Sjogren’s Syndrome
There are two primary types of Sjogren’s syndrome: primary and secondary.
Primary Sjogren’s Syndrome
This occurs in individuals who do not have any other autoimmune diseases. It is a standalone condition and typically manifests with dry eyes and mouth, though it may also affect other parts of the body.
Secondary Sjogren’s Syndrome
In this form, Sjogren’s occurs alongside another autoimmune disease, such as rheumatoid arthritis, lupus (systemic lupus erythematosus), or scleroderma. Patients with secondary Sjogren’s often experience more systemic involvement and complications due to the overlapping autoimmune disorders.
Epidemiology
Sjogren’s syndrome is relatively common among autoimmune disorders, affecting an estimated 0.1% to 4% of the population globally. However, because of under-diagnosis and the broad spectrum of symptoms, it is difficult to ascertain the exact prevalence. What is clear is that women are disproportionately affected, comprising about 90% of all diagnosed cases. The syndrome typically presents between the ages of 40 and 60, although it can affect individuals of any age, including children and young adults.
Causes of Sjogren’s Syndrome
The precise cause of Sjogren’s syndrome is not fully understood, but it is believed to result from a combination of genetic, environmental, and hormonal factors. These influences may include:
- Genetic Predisposition
- Environmental Triggers
- Hormonal Influences
- Autoimmune Dysregulation
Genetic Predisposition
Certain genetic markers have been associated with a higher risk of developing Sjogren’s syndrome, particularly in individuals who also have other autoimmune diseases. For example, genes related to the human leukocyte antigen (HLA) system, which is involved in immune regulation, are often implicated.
Environmental Triggers
Infections, particularly viral infections, may play a role in triggering Sjogren’s syndrome in genetically susceptible individuals. Epstein-Barr virus (EBV), cytomegalovirus (CMV), and hepatitis C have all been explored as potential triggers, though no single pathogen has been definitively linked to the disease.
Hormonal Influences
The vast majority of patients with Sjogren’s syndrome are female, leading researchers to investigate the role of sex hormones, particularly estrogen, in the development of the disease. While the exact mechanism is not clear, it is hypothesized that hormonal changes, such as those occurring during menopause, may contribute to the onset or worsening of symptoms.
Autoimmune Dysregulation
Like other autoimmune diseases, Sjogren’s syndrome is thought to involve a fundamental dysregulation of the immune system, wherein the body begins to target its own cells. In the case of Sjogren’s, this often involves the salivary and lacrimal glands, though other organs and systems may be involved.
Pathophysiology
The hallmark of Sjogren’s syndrome is lymphocytic infiltration of the exocrine glands, particularly the lacrimal and salivary glands. In a healthy individual, these glands produce saliva and tears, which are essential for maintaining the health of the mouth and eyes. However, in Sjogren’s syndrome, the immune system mistakenly targets these glands, leading to inflammation and reduced secretion.
Lymphocytes, particularly T and B cells, infiltrate the affected glands, resulting in tissue damage and dysfunction. Over time, this leads to chronic dryness, as the glands lose their ability to produce adequate moisture. In some patients, the immune attack extends beyond the exocrine glands, affecting organs such as the kidneys, lungs, liver, and nervous system, leading to more severe systemic complications.
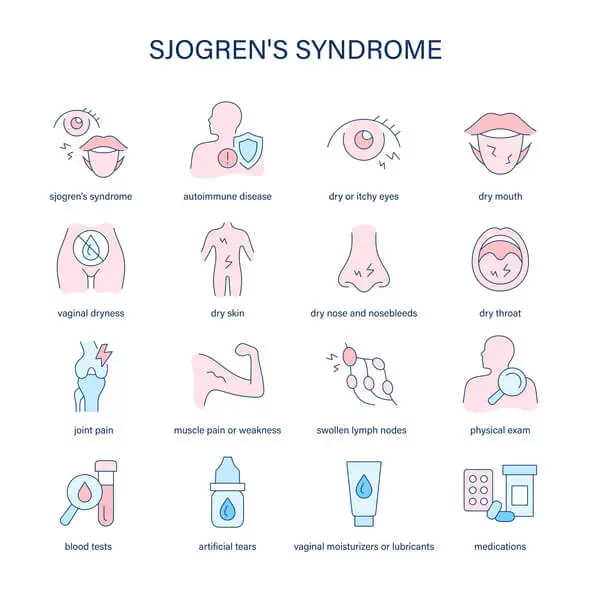
Symptoms of Sjogren’s Syndrome
Sjogren’s syndrome presents with a wide range of symptoms, varying from mild to severe. While the classic symptoms of dry mouth and dry eyes are the most common, the disease can affect multiple organs and systems, leading to a complex clinical picture.
Exocrine Gland Involvement
- Dry Mouth (Xerostomia)
- Dry Eyes (Keratoconjunctivitis Sicca)
- Dry Skin and Mucous Membranes
Dry Mouth (Xerostomia)
Reduced saliva production leads to difficulty chewing, swallowing, and speaking. Patients often report a burning sensation in the mouth and an increased susceptibility to dental caries, gum disease, and oral infections, such as candidiasis.
Dry Eyes (Keratoconjunctivitis Sicca)
Reduced tear production leads to irritation, a gritty sensation, redness, and sensitivity to light. If left untreated, chronic dryness can damage the cornea and lead to vision problems.
Dry Skin and Mucous Membranes
In addition to the eyes and mouth, dryness may affect the skin, nose, throat, and vagina, leading to discomfort and an increased risk of infection.
Systemic Involvement
Sjogren’s syndrome can extend beyond the exocrine glands, affecting various organs and systems:
- Joint Pain and Arthritis
- Fatigue
- Lung Involvement
- Kidney Involvement
- Peripheral Neuropathy
- Lymphoma
Joint Pain and Arthritis
Many patients with Sjögren’s experience joint pain and stiffness, similar to symptoms seen in rheumatoid arthritis. However, the joint involvement in Sjogren’s is usually less destructive.
Fatigue
Chronic fatigue is one of the most debilitating symptoms of Sjogren’s syndrome and can significantly impact quality of life. The fatigue experienced by patients is often profound, affecting daily functioning and leading to reduced productivity and social isolation.
Lung Involvement
Some patients develop interstitial lung disease (ILD), which causes inflammation and scarring of the lung tissue, leading to shortness of breath and a chronic cough. In severe cases, ILD can lead to respiratory failure.
Kidney Involvement
Sjogren’s can affect the kidneys, leading to conditions such as interstitial nephritis (inflammation of the kidney tissue) or renal tubular acidosis (an inability of the kidneys to maintain proper acid-base balance).
Peripheral Neuropathy
Some patients experience nerve damage, which can result in symptoms such as numbness, tingling, and pain, particularly in the hands and feet.
Lymphoma
Individuals with Sjogren’s syndrome are at an increased risk of developing non-Hodgkin’s lymphoma, particularly mucosa-associated lymphoid tissue (MALT) lymphoma. This risk is about 16 to 44 times higher than in the general population.
Diagnosis
Diagnosing Sjogren’s syndrome can be challenging due to the wide variability in symptoms and the overlap with other autoimmune diseases. Diagnosis typically involves a combination of clinical evaluation, laboratory tests, and imaging studies.
Clinical Evaluation
The doctor will take a detailed history and perform a physical examination, focusing on the presence of dry eyes and mouth, as well as any systemic symptoms. Special attention is given to the patient’s medical history, including the presence of other autoimmune diseases.
Laboratory Tests
- Autoantibodies
- Rheumatoid Factor (RF) and Antinuclear Antibodies (ANA)
- Salivary Gland Biopsy
- Schirmer’s Test
Autoantibodies
The presence of specific autoantibodies is a key diagnostic marker. Anti-Ro (SSA) and anti-La (SSB) antibodies are commonly found in patients with Sjogren’s syndrome, though their absence does not rule out the disease.
Rheumatoid Factor (RF) and Antinuclear Antibodies (ANA)
These are often elevated in patients with Sjogren’s syndrome, especially those with secondary Sjögren’s associated with rheumatoid arthritis or lupus.
Salivary Gland Biopsy
A minor salivary gland biopsy (usually taken from the lip) can reveal lymphocytic infiltration, which is a hallmark of the disease. This is particularly useful in patients with ambiguous symptoms or inconclusive blood tests.
Schirmer’s Test
This test measures tear production by placing a small strip of filter paper under the lower eyelid. Reduced tear production supports a diagnosis of Sjogren’s.
Imaging Studies
- Sialography
- Ultrasound or MRI of the Salivary Glands
Sialography
A specialized X-ray technique used to visualize the salivary glands and detect blockages or structural abnormalities.
Ultrasound or MRI of the Salivary Glands
These imaging techniques can help assess the size and structure of the salivary glands, identifying any inflammation or damage.
Treatment for Sjogren’s Syndrome
There is currently no cure for Sjogren’s syndrome, and treatment focuses on managing symptoms and preventing complications. The approach is often multidisciplinary, involving rheumatologists, ophthalmologists, dentists, and other specialists depending on the organs affected.
Symptomatic Treatment
- Dry Eyes
- Dry Mouth
- Oral Health
Dry Eyes
Artificial tears, lubricating ointments, and punctal plugs (small devices that block tear drainage) can help manage dry eyes. In more severe cases, prescription medications such as cyclosporine (Restasis) or lifitegrast (Xiidra) may be used to reduce inflammation and improve tear production.
Dry Mouth
Patients are advised to drink water frequently, chew sugar-free gum, and use saliva substitutes. Prescription medications such as pilocarpine (Salagen) or cevimeline (Evoxac) can stimulate saliva production.
Oral Health
Regular dental check-ups are essential for preventing cavities and gum disease. Fluoride treatments and antimicrobial mouthwashes can help protect against oral infections.
Systemic Treatment
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Immunosuppressive Medications
- Corticosteroids
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs may be used to relieve joint pain and inflammation, though they should be used cautiously due to the risk of gastrointestinal and cardiovascular side effects.
Immunosuppressive Medications
For patients with more severe systemic involvement, medications that suppress the immune system may be prescribed. These include hydroxychloroquine (Plaquenil), methotrexate, and biologics such as rituximab, which targets B cells involved in the autoimmune response.
Corticosteroids
In cases of organ involvement or severe systemic symptoms, corticosteroids may be used to reduce inflammation. However, long-term use is generally avoided due to the risk of side effects such as osteoporosis, weight gain, and increased infection risk.
Complications of Sjogren’s Syndrome
Sjogren’s syndrome can lead to a variety of complications, particularly when systemic involvement is present. The most common complications include:
- Infections
- Dental Issues
- Lymphoma
- Organ Damage
Infections
Dry mucous membranes increase the risk of infections, particularly in the eyes, mouth, and respiratory tract. Oral candidiasis and corneal ulcers are common complications.
Dental Issues
Reduced saliva production leads to an increased risk of dental caries and gum disease. Patients with Sjogren’s syndrome often require more frequent dental care.
Lymphoma
As mentioned earlier, patients with Sjogren’s syndrome have an increased risk of developing lymphoma, particularly MALT lymphoma. Early detection and treatment are critical in managing this complication.
Organ Damage
Systemic involvement can lead to damage in the kidneys, lungs, liver, and nervous system, depending on the organs affected.
Prognosis for Patients with Sjogren’s Syndrome
The prognosis for patients with Sjogren’s syndrome varies widely depending on the severity of the disease and the organs involved. Many patients with mild symptoms can manage the condition effectively with symptomatic treatment and regular medical care. However, those with systemic involvement or complications such as lymphoma may have a more guarded prognosis.
Chronic fatigue and pain are common challenges for patients with Sjogren’s syndrome, significantly affecting their quality of life. Moreover, the risk of developing other autoimmune diseases, such as lupus or rheumatoid arthritis, remains high for many patients.
Research and Future Directions
Despite significant advances in understanding Sjogren’s syndrome, many questions remain unanswered. Research is ongoing to better understand the underlying causes of the disease, identify more effective treatments, and improve diagnostic methods. Areas of interest include:
- Genetic Studies
- Biologic Therapies
- Stem Cell Therapy
Genetic Studies
Researchers are investigating the genetic factors that predispose individuals to Sjogren’s syndrome, with the hope of developing targeted therapies based on an individual’s genetic profile.
Biologic Therapies
The development of biologics that target specific components of the immune system has revolutionized the treatment of many autoimmune diseases. Ongoing research aims to identify new biologic treatments that can more effectively control the systemic inflammation seen in Sjogren’s syndrome.
Stem Cell Therapy
Experimental treatments involving stem cell therapy are being explored for their potential to repair damaged tissues and modulate the immune response in autoimmune diseases, including Sjogren’s syndrome.
Frequently Asked Questions (FAQs)
How is Sjogren’s syndrome diagnosed?
Diagnosis involves a combination of clinical evaluations and specialized tests. Doctors look for symptoms of dryness in the eyes and mouth and often use blood tests to check for specific autoantibodies (such as anti-Ro/SSA and anti-La/SSB). Additional assessments like the Schirmer test (to measure tear production) or a salivary gland biopsy may be performed to help confirm the diagnosis.
Does Sjogren’s get progressively worse?
The course of Sjogren’s syndrome varies from person to person. For some, symptoms remain relatively mild and stable over time, while others may experience a gradual worsening or more severe flare-ups. Regular follow-ups and personalized treatment plans are key to managing the condition and its progression.
What not to do with Sjogren’s?
While managing Sjogren’s syndrome often involves proactive lifestyle adjustments, it’s advisable to avoid factors that can exacerbate dryness or trigger flare-ups. This can include:
- Using medications that unnecessarily dry out the eyes or mouth (always consult your doctor before stopping any medications)
- Smoking and excessive alcohol consumption
- Neglecting proper hydration and oral care
Consulting with your healthcare provider can help you tailor lifestyle choices that minimize symptom triggers.
Can I live a normal life with Sjogren’s?
Yes, many individuals with Sjogren’s syndrome lead full and active lives. With appropriate treatment, regular medical care, and lifestyle modifications, most patients are able to manage their symptoms effectively and maintain a normal quality of life.
What is the lifespan of someone with Sjogren’s?
For most people, Sjogren’s syndrome does not significantly shorten life expectancy. The condition is generally managed with treatment and monitoring. However, some patients may develop complications or other autoimmune conditions that require careful management. Overall, with proper care, many individuals enjoy a normal lifespan.
What are the worst symptoms of Sjogren’s?
The severity of symptoms can differ among patients, but some of the most challenging issues include:
- Intense dryness of the eyes (which can lead to irritation or vision problems)
- Severe dry mouth (which can contribute to dental issues and difficulty swallowing)
- Persistent joint pain and fatigue
In some cases, other systemic complications—such as involvement of the kidneys, lungs, or nervous system—may occur, although these are less common.
What organ fails with Sjogren’s?
Sjogren’s syndrome primarily targets the glands that produce tears and saliva rather than causing a classic “organ failure.” That said, in some cases, the inflammatory process can affect other organs (such as the kidneys, lungs, or liver), leading to complications. However, outright organ failure is not typically characteristic of the syndrome.
Can Sjogren’s affect your legs?
Yes, Sjogren’s syndrome can affect the legs, usually indirectly. Some patients experience joint pain, muscle aches, or even peripheral neuropathy (nerve damage), which may lead to discomfort, weakness, or numbness in the legs. If you notice these symptoms, discussing them with your healthcare provider is important for appropriate management.
Conclusion
Sjogren’s syndrome is a complex autoimmune disease with a wide range of symptoms and potential complications. While dry eyes and dry mouth are the most recognizable features of the condition, it can affect multiple organ systems, leading to significant morbidity for some patients. Early diagnosis and a comprehensive, multidisciplinary approach to treatment are essential for managing the disease and improving the quality of life for those affected.
Ongoing research into the causes and treatment of Sjogren’s syndrome offers hope for more effective therapies in the future. Advances in biologic treatments and personalized medicine may eventually transform the landscape of care for patients with this challenging condition. For now, however, Sjogren’s syndrome remains a condition that requires vigilant management and a holistic approach to patient care.