Sinus perforation is a condition that can occur due to trauma, surgical complications, infections, or pathological processes, leading to a breach in the integrity of the sinus walls. The sinuses are air-filled cavities in the skull that play a significant role in respiratory function, voice resonance, and cranial weight reduction. When a sinus is perforated, it can lead to a range of symptoms, complications, and treatment challenges.
This article aims to provide an in-depth understanding of sinus perforation, its causes, clinical implications, and various treatment modalities.
Table of Contents
ToggleAnatomy of the Sinuses
The human skull houses four main pairs of sinuses:
- Maxillary Sinuses – Located in the cheekbones.
- Frontal Sinuses – Found in the forehead region.
- Ethmoidal Sinuses – Situated between the eyes.
- Sphenoidal Sinuses – Found deeper in the skull behind the ethmoidal sinuses.
Each sinus is lined with a mucous membrane and connected to the nasal cavity. The sinuses play a critical role in humidifying inhaled air, protecting the respiratory tract from pathogens, and enhancing the sense of smell.
Causes of Sinus Perforation
- Dental Procedures
- Trauma
- Surgical Complications
- Pathological Conditions
- Congenital Abnormalities
Dental Procedures
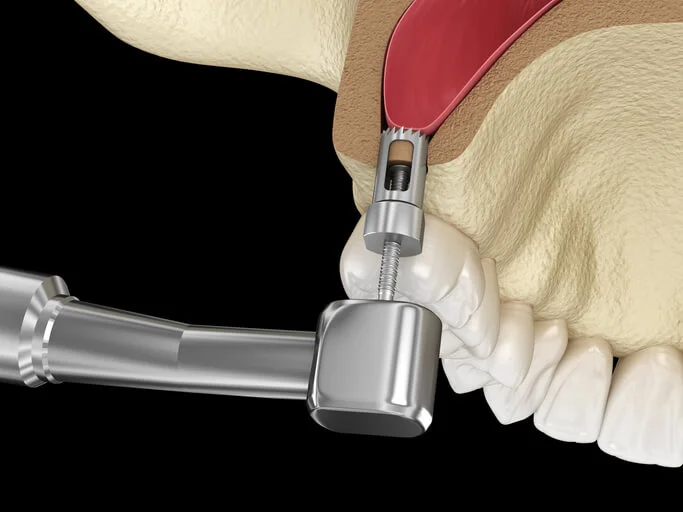
- Perforations often occur during tooth extractions, especially involving the upper molars or premolars, which are in close proximity to the maxillary sinus floor.
- Placement of dental implants can inadvertently breach the sinus floor.
Trauma
- Facial injuries from accidents or sports-related activities can lead to sinus perforation.
- Penetrating trauma can directly damage the sinus walls.
Surgical Complications
- Sinus surgeries, such as functional endoscopic sinus surgery (FESS) and sinus lift, can accidentally result in perforations.
- Complications from septoplasty or nasal reconstruction surgeries.
Pathological Conditions
- Chronic sinus infections or abscesses can erode sinus walls.
- Tumors, cysts, or other growths may invade the sinus cavity and compromise its structure.
Congenital Abnormalities
- In rare cases, developmental anomalies may predispose individuals to sinus perforation.
Symptoms of Sinus Perforation
The symptoms of sinus perforation vary depending on the location and severity of the perforation:
- Facial Pain or Pressure – Often localized near the affected sinus.
- Epistaxis (Nosebleeds) – Bleeding from the nasal cavity may occur.
- Nasal Congestion – Difficulty in breathing through the nose due to structural compromise.
- Air Escape During Speech or Sneezing – Known as “oroantral fistula” when perforation connects the oral cavity to the maxillary sinus.
- Recurrent Infections – Bacterial or fungal infections may become recurrent due to impaired sinus drainage.
- Altered Voice Resonance – Particularly in frontal or maxillary sinus perforations.
- Sinus Drainage into the Oral Cavity – This may occur if the maxillary sinus floor is perforated.
Diagnosis of Sinus Perforation
- Clinical Examination
- Radiographic Imaging
- Specialized Tests
Clinical Examination
- Thorough evaluation of symptoms and medical history.
- Inspection for signs of oroantral communication, swelling, or infection.
Radiographic Imaging
- X-rays – Useful for assessing bone integrity and sinus opacification.
- CT Scans – Provides detailed views of the sinus anatomy, perforation site, and surrounding structures.
- MRI – Beneficial for identifying soft tissue involvement or tumor-related causes.
Specialized Tests
- Valsalva maneuver may reveal air passage through the perforation.
- Dye or saline tests can help confirm oroantral fistulae.
Treatment Options for Sinus Perforation
- Non-Surgical Management
- Surgical Repair
- Management of Underlying Conditions
Non-Surgical Management
Small perforations, particularly those caused by trauma or minor dental procedures, may heal spontaneously with conservative treatment.
- Antibiotics – Prescribed to prevent secondary infections.
- Nasal Decongestants – Promote sinus drainage and reduce inflammation.
- Saline Irrigation – Helps maintain sinus hygiene and clear debris.
- Observation – Regular follow-ups to monitor healing.
Surgical Repair
When perforations fail to heal or result in significant symptoms, surgical intervention is often necessary. The choice of technique depends on the size, location, and cause of the perforation.
Oroantral Fistula Closure
Commonly performed for perforations involving the maxillary sinus floor.
Techniques include:
- Buccal Advancement Flap – A flap of mucosa from the cheek is advanced to cover the defect.
- Palatal Flap – A graft taken from the hard palate.
- Combined Approach – Buccal and palatal tissues are used together for large perforations.
- Collagen membranes or bone grafts may be added for structural support.
Endoscopic Sinus Surgery
- Utilized for repairing perforations in the ethmoid, sphenoid, or frontal sinuses.
- Minimally invasive techniques enable precise repair and restoration of sinus function.
Bone or Cartilage Grafting
- Grafts are often used for large perforations or when significant bone loss occurs.
- Common donor sites include the nasal septum, ear cartilage, or iliac crest.
Use of Synthetic Materials
Alloplastic materials, such as titanium mesh or bioresorbable plates, may be used for structural reconstruction.
Management of Underlying Conditions
In cases where perforation results from tumors, infections, or other pathologies, treating the underlying cause is critical.
For chronic infections, sinus drainage may be performed alongside defect repair.
Complications of Untreated Sinus Perforation
If left untreated, sinus perforation can lead to significant complications, including:
- Chronic Sinusitis – Persistent inflammation due to impaired drainage.
- Facial Cellulitis or Abscess – Infection spreading to surrounding tissues.
- Osteomyelitis – Bone infection, particularly in severe cases.
- Meningitis or Brain Abscess – Rare but serious complications when infection spreads intracranially.
Post-Treatment Care
- Medication
- Avoidance of Activities
- Follow-Up
Medication
Continued use of antibiotics and nasal decongestants as prescribed.
Avoidance of Activities
Patients should avoid blowing their nose, sneezing forcefully, or engaging in strenuous activities during the healing phase.
Follow-Up
Regular check-ups to monitor healing and address complications promptly.
Prevention of Sinus Perforation
- Careful surgical and dental techniques can minimize the risk of iatrogenic perforations.
- Early treatment of sinus infections and other conditions can prevent erosion of sinus walls.
- Protective gear during high-risk activities can reduce trauma-related perforations.
Frequently Asked Questions (FAQs)
How long does it take for a sinus perforation to heal?
The healing time for a sinus perforation depends on the size of the perforation, its cause, and the treatment method used.
- Small perforations: Minor perforations, such as those resulting from a simple dental extraction, may close within 2 to 6 weeks with proper care, including avoiding nose-blowing, sneezing forcefully, or using straws that create negative pressure.
- Moderate-sized perforations: These may take longer to heal and sometimes require surgical intervention if spontaneous healing does not occur.
- Large perforations or surgical repairs: If a surgical procedure, such as a buccal flap closure or bone graft, is performed, healing can take several months, with regular follow-ups needed to monitor recovery.
Patients should follow their dentist or ENT specialist’s instructions to ensure optimal healing and prevent complications such as infection or chronic sinusitis.
Can sinus perforations heal on their own?
Yes, sinus perforations can heal naturally, especially if they are small and not complicated by infection or excessive movement.
- Minor perforations (1-2 mm in size): Often heal spontaneously within a few weeks as long as the patient follows post-care instructions, such as avoiding excessive pressure on the affected area.
- Larger perforations (greater than 5 mm): May require surgical intervention, as the body may not be able to close the opening on its own.
- Factors that hinder healing: Poor oral hygiene, smoking, sinus infections, and excessive pressure changes (e.g., blowing the nose forcefully) can prevent natural healing.
If a perforation does not heal within a few weeks, a healthcare provider may recommend additional treatment.
What are the signs that my sinus perforation is getting worse?
If a sinus perforation does not heal properly, it can lead to complications. Some signs that the condition is worsening include:
- Persistent pain or pressure: Ongoing discomfort, particularly around the sinus region or affected tooth socket.
- Increased nasal discharge: A continuous runny nose or excessive drainage, especially if the fluid is yellow, green, or has a foul odor (a sign of infection).
- Foul smell and bad taste: This could indicate an infection or bacterial overgrowth in the sinus.
- Frequent nosebleeds: If blood is coming from the nose frequently, it could suggest irritation or a worsening of the perforation.
- Air escape during eating, drinking, or talking: Feeling air moving from the sinus into the mouth may indicate an oroantral fistula (a persistent hole between the oral cavity and sinus).
- Recurring sinus infections: If the sinus perforation remains open, bacteria can enter the sinus cavity, leading to chronic sinusitis with symptoms like headaches, nasal congestion, and facial pain.
If any of these symptoms occur, it’s important to consult a specialist for further evaluation and possible treatment.
Can I fly with a sinus perforation?
Flying with a sinus perforation is not recommended, especially if the perforation is recent or symptomatic.
- Cabin pressure changes: During takeoff and landing, changes in air pressure can cause discomfort or worsen symptoms due to the inability of the perforated sinus to equalize pressure properly.
- Increased pain and congestion: The perforation may lead to barotrauma, causing severe pressure-related pain, ear discomfort, and nasal congestion.
- Risk of infection: Exposure to dry cabin air and germs increases the likelihood of sinus infections.
If flying is necessary, the following precautions can help reduce discomfort:
- Use a nasal decongestant before flying to keep the nasal passages clear.
- Drink plenty of water to keep mucous membranes hydrated.
- Chew gum or yawn frequently to help equalize pressure.
- Consult a doctor before traveling to assess the severity of the perforation.
What foods should I avoid after sinus perforation repair?
After treatment for a sinus perforation, especially after oral surgery, it is important to avoid foods that could disrupt healing. Some foods to avoid include:
- Hard or crunchy foods: Chips, nuts, raw vegetables, and hard bread can irritate the wound and put pressure on the healing tissue.
- Sticky foods: Caramel, gum, or chewy candies can pull at the surgical site and increase the risk of opening the wound.
- Hot or spicy foods: Spicy meals can cause irritation, while very hot foods may slow the healing process.
- Dairy products (in some cases): Some dentists advise avoiding dairy products immediately after surgery, as they can thicken mucus and contribute to nasal congestion.
- Alcohol and carbonated drinks: These can cause irritation and dry out the mucous membranes.
- Straws and sucking actions: Avoid using straws, as the suction can dislodge blood clots and interfere with healing.
Instead, opt for soft foods such as yogurt, mashed potatoes, soups, smoothies (without straws), and well-cooked pasta until healing is well underway.
Will sinus perforation surgery leave a scar?
In most cases, sinus perforation surgery does not leave a visible scar because the procedure is performed inside the mouth or nasal passages.
- Buccal or palatal flaps used for repair are taken from inside the oral cavity and heal naturally over time without visible scarring.
- Endoscopic sinus surgery involves minimally invasive techniques, meaning there are no external incisions or scars.
- Bone grafting or synthetic materials used for larger defects integrate with surrounding tissues, leaving minimal to no noticeable signs after healing.
Although scarring inside the sinus or oral cavity can occur, it rarely causes significant long-term issues. However, some patients may experience mild changes in tissue texture or sensation.
Can a sinus perforation cause headaches?
Yes, a sinus perforation can contribute to headaches in several ways:
- Sinus pressure changes: A breach in the sinus can disrupt normal pressure regulation, leading to headaches.
- Inflammation and infection: If bacteria enter the sinus cavity through the perforation, it can lead to sinusitis, which often presents with headaches and facial pain.
- Nerve irritation: Some sinus perforations affect nearby nerves, leading to discomfort and headaches.
- Compromised sinus drainage: When normal mucus drainage is disrupted, it can cause congestion, pressure, and associated headaches.
If headaches persist after treatment, a specialist may evaluate whether additional therapy, antibiotics, or surgery is needed.
What happens if a sinus perforation is left untreated?
Leaving a sinus perforation untreated can lead to several complications:
- Persistent oroantral fistula (OAF): If the perforation remains open, it can develop into a chronic connection between the oral cavity and sinus, allowing food and fluids to pass into the sinus.
- Recurrent sinus infections: An open sinus can be an entry point for bacteria, leading to chronic sinusitis with ongoing congestion, headaches, and nasal discharge.
- Facial pain and pressure: The affected sinus may become inflamed or blocked, leading to pain, especially in the cheeks and forehead.
- Difficulty eating and speaking: Oroantral fistulas can cause discomfort while eating, drinking, or speaking, leading to air leakage and nasal regurgitation of fluids.
- Bone deterioration: In cases where a sinus perforation occurs due to dental procedures, leaving it untreated may contribute to bone loss in the jaw, affecting future dental treatments such as implants.
If a perforation does not heal within a few weeks, surgical intervention may be required to close the defect and prevent complications.
Conclusion
Sinus perforation is a condition that requires prompt recognition and tailored management to prevent complications and restore normal sinus function. While small perforations may heal spontaneously, surgical intervention is often necessary for larger defects or those associated with recurrent infections.
Advances in imaging, surgical techniques, and biomaterials have significantly improved outcomes for patients with sinus perforations. Multidisciplinary care involving otolaryngologists, oral surgeons, and radiologists is often essential for successful treatment.
Early diagnosis and proactive treatment remain the cornerstone of effective management, ensuring optimal recovery and minimizing long-term complications.