Conventional dental implants typically require a substantial amount of alveolar bone for placement, which can be problematic for patients with severe bone resorption. Traditionally, such cases required extensive bone grafting procedures before implant placement. However, the advent of short dental implants offers an alternative solution with fewer surgical demands and shorter treatment times.
Short implants are defined by their reduced length generally less than 8 mm. Their design and use have evolved significantly over the past two decades, supported by improvements in implant materials, surface modifications, and surgical techniques. Despite earlier skepticism due to concerns about reduced bone-implant contact and mechanical stability, modern short implants now demonstrate promising success rates and clinical performance.
This article provides an in-depth overview of short implants, exploring their indications, biomechanical considerations, clinical success, advantages, disadvantages, and evidence-based outcomes.
Table of Contents
ToggleWhat Are Short Dental Implants?
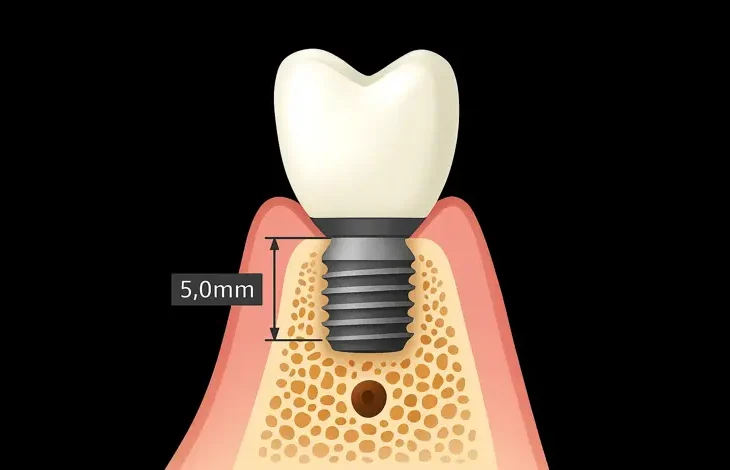
There is some variability in the literature regarding the precise definition of short implants. Most studies and clinicians define short implants as those with an intraosseous length of less than 8 mm, with some suggesting “ultra-short” implants for lengths ≤6 mm.
Design Characteristics
Short implants are not simply shorter versions of conventional implants. To compensate for their reduced length, manufacturers often incorporate design modifications such as:
- Increased diameter to provide greater surface area.
- Enhanced surface treatments for improved osseointegration.
- Aggressive thread designs for better primary stability.
- Platform switching to reduce crestal bone loss.
Indications for Short Implants
Short implants are primarily indicated in areas with reduced vertical bone height, where bone augmentation procedures would otherwise be required. Common scenarios include:
- Posterior maxilla with proximity to the maxillary sinus.
- Posterior mandible with proximity to the inferior alveolar nerve.
- Patients unwilling or unable to undergo bone grafting due to medical, financial, or personal reasons.
- Elderly patients or those with systemic conditions that contraindicate extensive surgery.
Biomechanical Considerations
Bone-to-Implant Contact (BIC)
One of the main concerns with short implants is the reduced bone-implant interface. The lower surface area can potentially compromise primary stability and increase stress concentration. However, modern surface treatments such as sandblasting, acid-etching, and plasma spraying enhance osseointegration even in short fixtures.
Crown-to-Implant Ratio
Short implants often have a high crown-to-implant ratio (CIR), especially in cases of vertical bone loss. Although historically this was seen as a risk factor for mechanical complications, studies show that with proper occlusal management and splinting strategies, even high CIRs can be successfully managed.
Occlusal Load Management
To ensure the longevity of short implants, occlusal forces must be carefully controlled. This includes:
- Using splinted restorations to distribute forces.
- Avoiding cantilever designs.
- Employing mutually protected occlusion.
- Managing parafunctional habits such as bruxism.
Surgical Protocols
The placement of short implants follows similar surgical protocols to conventional implants, with some adjustments:
- Preoperative Planning: 3D imaging and digital planning are crucial for assessing bone availability and anatomical constraints.
- Site Preparation: Minimally traumatic drilling and under-preparation of the osteotomy site enhance primary stability.
- Placement Techniques: Guided surgery can improve precision, especially in compromised sites.
- Loading Protocols: Depending on primary stability, either immediate or delayed loading can be considered.
Clinical Performance and Success Rates
Success Criteria
The success of short implants is evaluated based on:
- Osseointegration and absence of mobility.
- Lack of peri-implant radiolucency.
- Marginal bone loss <1.5 mm in the first year.
- Absence of persistent pain or infection.
Success Rates Compared to Standard Implants
Earlier studies expressed concern over the predictability of short implants. However, modern meta-analyses and long-term studies show comparable survival rates to conventional implants:
- A systematic review by Thoma et al. (2018) showed a 5-year survival rate of over 95% for short implants.
- The ITI Consensus Report (2018) endorsed short implants as a reliable alternative in posterior regions.
Performance in the Maxilla vs. Mandible
Historically, short implants performed better in the mandible due to denser bone. However, improvements in surface technology have mitigated this difference. In both jaws, bone quality and primary stability remain important determinants of success.
Advantages of Short Implants
- Avoidance of Bone Grafting: Eliminates need for sinus lift, ridge augmentation, or nerve repositioning. Also reduces surgical complexity, cost, and morbidity.
- Shorter Treatment Time: Fewer surgical steps mean faster treatment completion.
- Reduced Risk of Complications: Less invasive procedures decrease the risk of nerve injury and sinus perforation.
- Cost-Effective: Lower material and surgical costs make treatment more affordable.
- Patient Acceptability: Less invasive protocols are more acceptable to patients wary of extensive surgery.
Limitations and Challenges
- Biomechanical Limitations: Greater stress concentration due to reduced surface area. Higher risk of mechanical failure if occlusal forces are not controlled.
- High Crown-to-Implant Ratios: May lead to unfavorable load distribution and marginal bone loss if not properly managed.
- Limited Long-Term Data: Although current data are promising, more long-term (>10 years) studies are needed.
- Not Suitable for All Cases: Severely atrophic jaws with compromised horizontal bone may still require augmentation.
Clinical Case Selection and Treatment Planning
Successful use of short implants requires careful case selection and meticulous planning:
- Assess Bone Volume: Use CBCT to evaluate vertical and horizontal bone dimensions.
- Evaluate Occlusal Scheme: Consider occlusal forces, parafunction, and prosthetic requirements.
- Medical Assessment: Ensure systemic health allows for osseointegration and healing.
- Patient Expectations: Discuss pros and cons, and align treatment goals with patient priorities.
Prosthetic Considerations
Restorations on short implants should be carefully designed to minimize complications:
- Splinting Adjacent Implants: Especially in posterior regions, splinting reduces micromovement and distributes stress.
- Screw-Retained Crowns: Allow easier retrieval and reduce cement-associated peri-implantitis risk.
- Use of Angulated Abutments: In cases with anatomical constraints, angulated abutments help optimize prosthetic emergence.
- Material Selection: Use high-strength ceramics or metal-ceramic restorations for posterior load-bearing areas.
Comparison with Bone Augmentation Techniques
| Aspect | Short Implants | Bone Augmentation + Standard Implants |
|---|---|---|
| Invasiveness | Minimally invasive | Highly invasive |
| Treatment Duration | Shorter | Longer |
| Cost | Lower | Higher |
| Complication Risk | Lower (e.g., no sinusitis, paresthesia) | Higher (e.g., graft failure, infection) |
| Predictability | High in selected cases | High with experienced surgeons |
Short implants offer a pragmatic solution for patients who are not ideal candidates for bone augmentation or those seeking a simpler and quicker treatment modality.
Conclusion
Short dental implants have emerged as a viable and effective option for treating edentulous spaces in areas with limited bone height. With improved design, surface technology, and surgical protocols, short implants now demonstrate clinical outcomes comparable to conventional implants, especially when placed in properly selected cases.
They offer multiple benefits, including reduced treatment time, avoidance of grafting, lower cost, and higher patient acceptance. However, successful outcomes depend on a thorough understanding of biomechanical principles, careful treatment planning, and proper prosthetic execution.
As the field continues to evolve, short implants are likely to play an increasingly important role in mainstream implant dentistry, offering clinicians a versatile tool to meet the diverse needs of their patients.