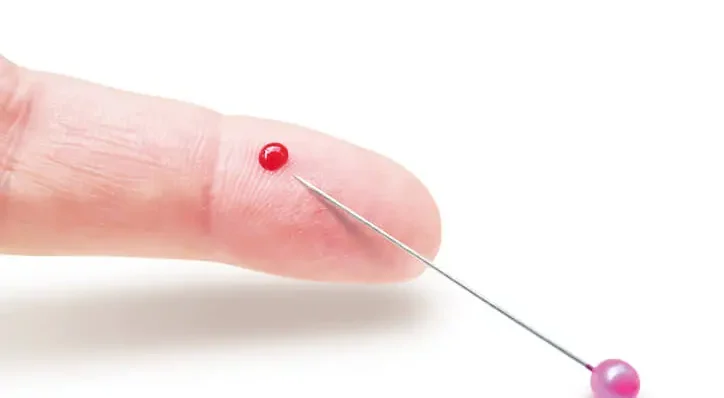
Needle stick injuries (NSIs) represent a significant occupational hazard in the healthcare industry, including dentistry. Dental professionals, including dentists, dental hygienists, and assistants, are at considerable risk due to the nature of their work which involves the use of sharp instruments, needles, and close contact with patients. This article explores the prevalence, risks, prevention strategies, and management of needle stick injuries among dental professionals.
Table of Contents
TogglePrevalence of Needle Stick Injuries in Dentistry
NSIs are common in dental practices due to the frequent use of needles for local anesthesia, suturing, and other procedures. Studies indicate that the prevalence of NSIs among dental professionals is alarmingly high. A survey conducted among dental practitioners revealed that a significant percentage reported experiencing at least one NSI in their career. Dental assistants and hygienists are also susceptible due to their involvement in handling sharps and contaminated instruments.
The high prevalence of NSIs in dentistry can be attributed to various factors such as:
- Frequent Use of Needles
- Close Proximity to Patients
- High Volume of Patients
- Inadequate Training and Safety Protocols
Frequent Use of Needles
Procedures like administering local anesthesia require the frequent use of needles.
Close Proximity to Patients
The close quarters in which dental professionals work increase the risk of accidental sticks.
High Volume of Patients
Busy dental practices may lead to rushed procedures, increasing the likelihood of NSIs.
Inadequate Training and Safety Protocols
Lack of proper training in handling sharps and insufficient safety measures contribute to the risk.
Risks Associated with Needle Stick Injuries
NSIs pose significant health risks primarily due to the potential transmission of blood-borne pathogens such as Hepatitis B (HBV), Hepatitis C (HCV), and Human Immunodeficiency Virus (HIV). These pathogens can lead to serious, chronic health conditions, and in some cases, be life-threatening.
Transmission Risks
- Hepatitis B
- Hepatitis C
- HIV
Hepatitis B
HBV is highly infectious and can survive outside the body for up to a week. The risk of transmission from a needle stick injury involving an HBV-positive patient is approximately 6-30%.
Hepatitis C
HCV transmission risk from a needle stick injury is about 1.8%. Unlike HBV, there is no vaccine for HCV, making prevention crucial.
HIV
The risk of HIV transmission from a needle stick injury is approximately 0.3%. While lower than HBV and HCV, the impact of HIV infection is significant due to the chronic nature of the disease and the current lack of a cure.
Psychological Impact
Apart from physical health risks, NSIs can also have profound psychological effects on dental professionals. Anxiety and stress related to the fear of contracting infections can affect their mental health and job performance. The stigma associated with blood-borne diseases can also lead to social and professional isolation.
Prevention Strategies
Preventing NSIs requires a comprehensive approach that includes proper training, the implementation of safety protocols, and the use of safety-engineered devices. Here are some key strategies for preventing NSIs in dental settings:
- Education and Training
- Safety Protocols and Best Practices
- Use of Safety-Engineered Devices
Education and Training
Continuous education and training are essential for all dental staff. Training should focus on:
- Proper Handling of Needles and Sharps
- Use of Safety Devices
- Post-Exposure Protocols
Proper Handling of Needles and Sharps
Techniques for safe handling, disposal, and management of needles should be regularly reinforced.
Use of Safety Devices
Training on the correct use of safety-engineered devices such as retractable needles and needle guards.
Post-Exposure Protocols
Ensuring that all staff are aware of the steps to take following a needle stick injury to minimize health risks.
Safety Protocols and Best Practices
Adopting stringent safety protocols can significantly reduce the risk of NSIs. Best practices include:
- No Recapping of Needles
- Sharps Disposal Containers
- Personal Protective Equipment (PPE)
- Safe Work Environment
No Recapping of Needles
Avoiding the recapping of needles or using one-handed recapping techniques if absolutely necessary.
Sharps Disposal Containers
Utilizing clearly marked and puncture-resistant sharps containers located at the point of use.
Personal Protective Equipment (PPE)
Wearing appropriate PPE such as gloves, masks, and eye protection to reduce exposure risk.
Safe Work Environment
Ensuring adequate lighting, reducing clutter, and organizing the workspace to minimize accidental injuries.
Use of Safety-Engineered Devices
Advancements in technology have led to the development of safety-engineered devices designed to reduce the risk of NSIs. These include:
- Retractable Needles
- Needle Guards
- Blunt-Tip Needles
Retractable Needles
Needles that retract into the syringe barrel after use, preventing accidental sticks.
Needle Guards
Protective devices that cover the needle after use.
Blunt-Tip Needles
Used for certain procedures to reduce the risk of injury.
Management of Needle Stick Injuries
Despite best efforts, NSIs can still occur. Proper management of these injuries is crucial to minimize health risks and ensure the well-being of dental professionals. The management of NSIs involves immediate actions, post-exposure prophylaxis (PEP), and follow-up procedures.
Immediate Actions
Immediate steps following a needle stick injury include:
- Encourage Bleeding
- Clean the Wound
- Report the Incident
Encourage Bleeding
Allow the wound to bleed freely but do not squeeze or scrub the area.
Clean the Wound
Wash the area thoroughly with soap and water. Use antiseptics if available.
Report the Incident
Inform the designated safety officer or supervisor about the injury immediately.
Post-Exposure Prophylaxis (PEP)
PEP involves the administration of medications to prevent infection after exposure to a blood-borne pathogen. The steps include:
- Risk Assessment
- Testing
- Medication
Risk Assessment
Evaluating the risk based on the type of exposure, the health status of the source patient, and the injured person’s health status.
Testing
Baseline testing for HBV, HCV, and HIV for both the source patient and the injured person.
Medication
If the source patient is known to be HIV positive, antiretroviral therapy should be started as soon as possible, ideally within hours of exposure. For HBV, vaccination and/or HBV immune globulin may be administered.
Follow-Up Procedures
Ongoing monitoring and follow-up are essential to ensure that no infection develops post-exposure. This includes:
- Repeat Testing
- Counseling and Support
- Documentation and Review
Repeat Testing
Follow-up testing for HIV, HBV, and HCV at recommended intervals (e.g., 6 weeks, 3 months, and 6 months post-exposure).
Counseling and Support
Providing psychological support and counseling for the affected individual.
Documentation and Review
Keeping detailed records of the incident, the response, and the outcomes. Reviewing the incident to identify potential improvements in safety protocols.
Frequently Asked Questions (FAQs)
What is the most common needle stick injury?
The most common needle stick injury occurs when a healthcare worker accidentally punctures their skin with a contaminated needle. These injuries frequently happen during medical procedures such as administering injections, drawing blood, or handling sharp instruments. Needle stick injuries are also common during improper disposal of needles or when recapping used needles. These incidents pose a serious risk of exposure to bloodborne pathogens such as HIV, Hepatitis B (HBV), and Hepatitis C (HCV).
What is the correct procedure if you get a needle stick injury?
If you sustain a needle stick injury, it is crucial to act immediately:
- Wash the wound: Rinse the puncture site with soap and water. Avoid scrubbing, as it may cause further tissue damage.
- Encourage bleeding: Let the wound bleed slightly to help flush out contaminants, but do not forcefully squeeze the area.
- Apply antiseptic: Use an antiseptic solution, such as iodine or alcohol, to disinfect the affected area.
- Cover the wound: Protect the wound with a sterile bandage to prevent infection.
- Report the injury: Notify your supervisor or occupational health department immediately.
- Seek medical attention: Undergo a risk assessment to determine the necessity of post-exposure prophylaxis (PEP) for potential infections.
What are the 5 steps to follow immediately after an accidental needle stick injury?
- Step 1: Clean the wound – Wash the site with soap and water. Avoid using harsh chemicals or scrubbing excessively.
- Step 2: Allow minimal bleeding – Let the wound bleed slightly but avoid squeezing, as it could drive pathogens deeper into the tissue.
- Step 3: Apply antiseptic – Use disinfectant solutions such as alcohol or iodine to reduce the risk of infection.
- Step 4: Report the incident – Inform your employer or designated health officer as per workplace protocols.
- Step 5: Seek medical evaluation – A healthcare provider will assess the risk of transmission and may recommend post-exposure prophylaxis (PEP) or follow-up testing.
What is the policy for needle stick injury?
Policies regarding needle stick injuries vary by institution but typically include the following:
- Mandatory reporting of all needle stick injuries.
- Immediate first aid procedures for exposed individuals.
- Risk assessment based on the source patient’s medical history and test results.
- Medical evaluation and potential administration of post-exposure prophylaxis (PEP) to prevent infection.
- Documentation of the incident and investigation into preventative measures to reduce future occurrences.
- Training programs to educate healthcare workers on safe handling and disposal of needles.
What is the protocol for a needlestick?
The protocol for a needle stick injury includes:
- Immediate first aid treatment, including washing the wound and applying antiseptic.
- Reporting the injury to an employer, supervisor, or occupational health service.
- Assessing the risk of bloodborne pathogen exposure by evaluating the source of the contaminated needle.
- Testing and monitoring both the injured individual and, if possible, the source patient.
- Receiving necessary treatment, including vaccination for Hepatitis B or post-exposure prophylaxis (PEP) for HIV.
- Following up with additional testing at intervals to ensure no infection has occurred.
What are the odds of getting a disease from a needlestick?
The risk of infection depends on several factors, including the pathogen present, the depth of the injury, and the amount of blood transferred. The estimated risk of transmission from a contaminated needle is:
- HIV: 0.3% (3 in 1,000 cases)
- Hepatitis B (HBV): Up to 30% if unvaccinated
- Hepatitis C (HCV): Approximately 1.8% These risks are significantly reduced with proper post-exposure prophylaxis and vaccinations.
How long after a needlestick should I get tested?
Testing schedules vary depending on the pathogen:
- HIV: Initial test at exposure, followed by testing at 6 weeks, 3 months, and 6 months.
- Hepatitis B and C: Baseline test at exposure, then follow-up tests at 6 weeks, 3 months, and 6 months. Early testing ensures timely detection and intervention if necessary.
What is the highest rate of infection from needle stick?
The highest risk of infection comes from Hepatitis B (HBV), with transmission rates as high as 30% if the exposed individual is not vaccinated. This is followed by Hepatitis C (HCV) at approximately 1.8% and HIV at 0.3%. Vaccination against Hepatitis B and prompt post-exposure interventions significantly reduce these risks.
Do needlestick injuries need to be reported?
Yes, all needlestick injuries must be reported immediately. Reporting ensures:
- Proper medical evaluation and timely intervention.
- Prevention of further exposure to the injured worker and colleagues.
- Compliance with workplace safety protocols and regulatory requirements.
Data collection for institutional safety improvements and risk reduction strategies. Failing to report a needlestick injury may delay necessary treatments and increase the risk of infection.
Conclusion
Needle stick injuries pose a serious threat to dental professionals, both in terms of physical health risks and psychological impact. The high prevalence of these injuries in dental settings necessitates a multifaceted approach to prevention, incorporating education, safety protocols, and the use of advanced safety devices. In the event of an NSI, prompt and effective management is crucial to minimize health risks. By fostering a culture of safety and vigilance, the dental profession can better protect its members from the dangers of needle stick injuries and ensure a safer working environment for all.