Herpes simplex virus (HSV) is a widespread viral infection that affects millions of people worldwide. It belongs to the Herpesviridae family and is classified into two main types: HSV-1, which is primarily associated with oral herpes, and HSV-2, which is more commonly linked to genital herpes. Despite its prevalence, HSV remains a misunderstood and often stigmatized condition. This article explores HSV’s biology, transmission, symptoms, treatment, and ongoing research, providing a comprehensive understanding of the virus.
HSV infections have been documented for centuries, with references dating back to ancient Greece and Rome. The virus’s ability to remain dormant in the nervous system and reactivate intermittently makes it a lifelong condition for those infected. With an estimated 3.7 billion people under the age of 50 having HSV-1 and over 400 million affected by HSV-2, understanding and managing the virus is crucial for public health.
Table of Contents
ToggleTypes of Herpes Simplex Virus
HSV-1 (Oral Herpes)
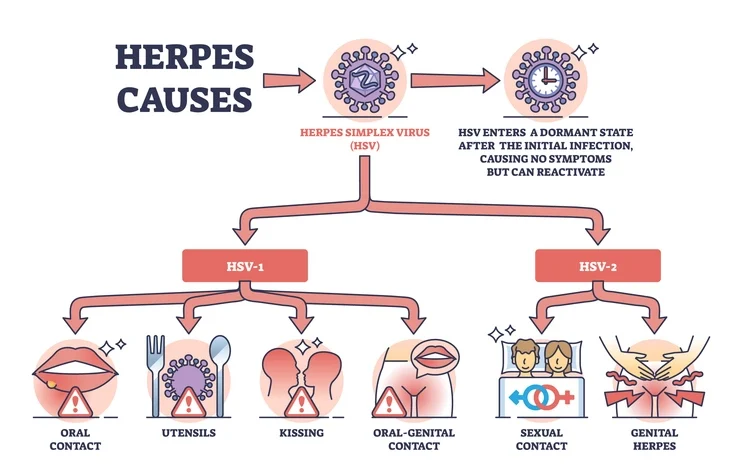
HSV-1 is commonly transmitted through direct contact with infected saliva or skin. It is primarily responsible for oral herpes, which manifests as cold sores or fever blisters around the mouth and lips. However, HSV-1 can also cause genital herpes through oral-genital contact.
In addition to cold sores, HSV-1 can sometimes lead to more severe conditions such as herpetic whitlow (a painful infection on the fingers), herpes keratitis (eye infections that can lead to vision problems), and herpes gladiatorum (common in athletes, particularly wrestlers, due to skin-to-skin contact).
HSV-2 (Genital Herpes)
HSV-2 is primarily transmitted through sexual contact and is the leading cause of genital herpes. This type of herpes results in painful sores and blisters around the genital and anal areas. Although less common, HSV-2 can also infect the mouth through oral-genital exposure.
HSV-2 infections often lead to recurring outbreaks, particularly in individuals with weakened immune systems. Women are more likely to be infected with HSV-2 than men, and the virus poses significant risks for pregnant women and newborns.
Transmission of HSV
HSV spreads through direct contact with infected skin, saliva, or bodily fluids. The virus is most contagious when active sores are present, but it can also be transmitted when there are no visible symptoms due to asymptomatic viral shedding.
Common modes of transmission include:
- Kissing (HSV-1, particularly among children and close family members)
- Sharing utensils, drinking glasses, or personal items (HSV-1)
- Oral-genital contact (HSV-1 or HSV-2)
- Sexual intercourse (vaginal, anal, or oral) (HSV-2 and sometimes HSV-1)
- Mother-to-child transmission during childbirth (Neonatal herpes, which can be severe)
- Skin-to-skin contact in sports (e.g., wrestlers developing herpes gladiatorum)
Because HSV can be transmitted without visible symptoms, many individuals unknowingly spread the virus. Education about safe practices and preventive measures is essential in reducing HSV transmission rates.
Symptoms of HSV Infection
The symptoms of HSV infection vary in severity and may differ between primary and recurrent infections.
Primary Infection
The first outbreak of HSV is usually more severe than subsequent recurrences. Symptoms appear within 2 to 12 days of exposure and may include:
- Painful blisters or sores on the affected area
- Flu-like symptoms such as fever, body aches, and swollen lymph nodes
- Pain or difficulty while urinating (especially with genital herpes)
- Tingling or burning sensation before sores appear
- Increased fatigue and general discomfort
- Headaches and muscle pain
Recurrent Infections
After the primary infection, HSV remains dormant in the body and can reactivate later. Triggers for reactivation include stress, illness, hormonal changes, and a weakened immune system. Recurrent outbreaks are usually less severe and shorter in duration.
Asymptomatic Infections
Many people with HSV experience no symptoms or have very mild ones that go unnoticed. Despite this, they can still transmit the virus to others.
Diagnosis of HSV
Diagnosing HSV involves several methods, including:
- Physical examination: A doctor may diagnose herpes by observing sores.
- Polymerase Chain Reaction (PCR) test: Detects HSV DNA in a sample taken from a sore or blood.
- Viral culture: A sample from a sore is tested for the presence of HSV.
- Blood tests: Detect antibodies for HSV-1 and HSV-2, indicating past or current infection.
Early diagnosis is essential in managing the condition and preventing the spread of the virus.
Treatment and Management
There is no cure for HSV, but antiviral medications help manage symptoms and reduce the risk of transmission.
Antiviral Medications
Common antiviral drugs include:
- Acyclovir (Zovirax): Reduces symptoms and speeds up healing time.
- Valacyclovir (Valtrex): Helps suppress outbreaks and lowers transmission risk.
- Famciclovir (Famvir): Often used for severe or frequent outbreaks.
Home Remedies and Lifestyle Changes
- Keeping sores clean and dry to prevent secondary infections.
- Applying cold compresses to relieve pain and inflammation.
- Using over-the-counter pain relievers like ibuprofen or acetaminophen.
- Avoiding triggers such as stress, sun exposure, and lack of sleep.
Suppressive Therapy
For individuals with frequent outbreaks, daily antiviral medication can reduce recurrence and decrease transmission risks to partners.
HSV and Pregnancy
Pregnant women with HSV require special care to prevent neonatal herpes, a serious condition that can be fatal to newborns. If a woman has an active outbreak near delivery, doctors may recommend a C-section to prevent transmission.
Complications of HSV
While HSV is generally not life-threatening, it can lead to severe complications in some cases:
- Neonatal herpes: Can cause severe neurological damage or death in newborns.
- Herpetic encephalitis: A rare but serious infection of the brain caused by HSV.
- Increased HIV risk: HSV-2 infection increases susceptibility to HIV.
- Psychological impact: The stigma surrounding herpes can cause emotional distress and anxiety.
Prevention of HSV
While there is no vaccine for HSV, several preventive measures can help reduce the risk of infection:
- Using condoms or dental dams during sexual activity.
- Avoiding sexual contact during outbreaks.
- Taking antiviral medication if prescribed for suppressive therapy.
- Practicing good hygiene by avoiding sharing personal items like lip balms and razors.
Ongoing Research and Future Developments
Research is ongoing to develop better treatments and vaccines for HSV. Some promising areas include:
- HSV vaccines: Scientists are working on vaccines to prevent or reduce the severity of HSV infections.
- CRISPR gene-editing: A potential method to remove HSV from infected cells.
- New antiviral drugs: More effective and longer lasting treatments are being explored.
Frequently Asked Questions (FAQs)
Is HSV a big deal?
HSV (herpes simplex virus) is very common, and while it can be emotionally challenging due to stigma, it is not a serious medical condition for most people. Millions of people worldwide have herpes, and the majority experience mild symptoms or none at all. The virus does not lead to life-threatening health complications in otherwise healthy individuals. However, it is a lifelong condition, so managing it with antiviral medications, healthy habits, and communication in relationships is important. The biggest challenge for most people is not the physical symptoms but the social stigma surrounding herpes.
Can a person with herpes live a normal life?
Absolutely. Having herpes does not stop anyone from having a fulfilling romantic life, a successful career, or even having children. Many people with herpes go on to have healthy relationships and families. The virus can be managed with antiviral medications that reduce outbreaks and lower the risk of transmission. Many people only have occasional outbreaks, while others may never experience noticeable symptoms after their initial outbreak. As long as precautions are taken and communication is open in relationships, herpes does not have to significantly impact a person’s daily life.
What triggers a herpes outbreak?
Herpes outbreaks can be triggered by several factors, including:
- Stress: High levels of emotional or physical stress can weaken the immune system, making outbreaks more likely.
- Illness: A cold, flu, or other infections can make the body more vulnerable to an outbreak.
- Fatigue: Lack of sleep or overexertion can lower the body’s ability to suppress the virus.
- Hormonal changes: Some people, particularly women, may notice outbreaks around menstruation due to hormonal fluctuations.
- Friction or irritation: Sexual activity, tight clothing, or excessive sun exposure (especially for oral herpes) can trigger an outbreak.
- Weakened immune system: Conditions that affect immunity, such as autoimmune diseases or chemotherapy, can make outbreaks more frequent.
Managing stress, maintaining a healthy lifestyle, and taking antiviral medication if needed can help minimize outbreaks.
What do I do if I have HSV-1?
If you have HSV-1 (which commonly causes oral herpes but can also affect the genitals), here are some steps you can take:
- Educate yourself: Learn about the virus to separate myths from facts. HSV-1 is extremely common and not a serious health risk for most people.
- Practice good hygiene: Avoid touching an active cold sore and wash your hands frequently to prevent spreading the virus to other areas of your body or other people.
- Avoid close contact during outbreaks: HSV-1 is most contagious when sores are present. Avoid kissing or oral sex during this time.
- Consider antiviral medication: If you experience frequent outbreaks, a doctor may prescribe antivirals like acyclovir or valacyclovir to reduce symptoms and transmission risk.
- Maintain a healthy immune system: Eat well, get enough sleep, and manage stress to help reduce outbreaks.
- Communicate with partners: If you’re in a relationship, be open about your diagnosis and discuss ways to reduce transmission risks.
Should I date someone with herpes?
Yes, you can date someone with herpes without it being a major concern. Herpes is a manageable condition, and many couples navigate it successfully. Here’s what to keep in mind:
- Education helps: Understanding how herpes works can eliminate unnecessary fears. It is a common and manageable virus.
- Precautions reduce risk: Using condoms and dental dams, avoiding contact during outbreaks, and considering antiviral medication can greatly reduce the chance of transmission.
- Open communication builds trust: A partner with herpes who is upfront and educated about their condition is likely responsible and considerate in relationships.
- The stigma is worse than the condition: Most people with herpes live completely normal lives, and the virus does not define them.
If you have concerns, discussing them openly with your partner and possibly consulting a healthcare provider together can help ease any worries.
What’s the worst thing about having herpes?
For most people, the worst part about herpes is the stigma, not the physical symptoms. While the virus can cause outbreaks that may be uncomfortable, these tend to be mild and become less frequent over time. In fact, many people with herpes never experience noticeable symptoms.
The emotional burden—fear of judgment, rejection, or misinformation—can be more difficult to deal with than the virus itself. However, as more people become educated, the stigma is slowly fading. Many people in relationships find that herpes does not significantly impact their lives once they understand how to manage it.
Can you sleep with someone with herpes and not get it?
Yes, it is possible to have a sexual relationship with someone who has herpes and never contract the virus. The risk of transmission depends on several factors:
- Antiviral medication: If the partner with herpes takes daily antiviral medication (such as valacyclovir), the risk of transmission drops significantly.
- Use of protection: Condoms and dental dams reduce skin-to-skin contact and lower the chance of spreading the virus.
- Avoiding sexual contact during outbreaks: Herpes is most contagious when sores are present, so abstaining from sex during an outbreak is crucial.
- Asymptomatic shedding: The virus can be transmitted even when no symptoms are visible, but shedding occurs less frequently when the infected partner is on antiviral medication.
By following these precautions, many couples successfully prevent transmission.
Is herpes the worst STD to have?
No, herpes is not the worst STD. While it is a lifelong condition, it is not life-threatening and does not cause serious health complications in most people. Other STDs, such as HIV, syphilis (if untreated), and HPV (which can lead to cancer), have far more severe consequences.
Herpes primarily causes mild skin irritation and occasional outbreaks, but it does not damage organs, lead to infertility, or affect long-term health. The worst part about herpes is often the stigma, which is based on misconceptions rather than medical facts.
Does HSV-1 mean my partner cheated?
Not necessarily. HSV-1 is extremely common and is often contracted through non-sexual means, such as kissing family members during childhood. Many people have HSV-1 for years without knowing, as it can remain dormant without causing noticeable symptoms.
If your partner is diagnosed with HSV-1, it does not automatically mean they were unfaithful. They may have had the virus before your relationship, or they could have acquired it from an innocent, non-sexual interaction. The best way to approach this situation is through open and honest communication rather than jumping to conclusions.