Modern dentistry increasingly relies on biochemical agents to complement mechanical procedures, especially in endodontics. Among these agents, EDTA (Ethylenediaminetetraacetic acid) stands out for its ability to dissolve inorganic materials and modify the dentin substrate. First introduced into dentistry in the mid-20th century, EDTA’s use has become routine in endodontic treatment due to its powerful chelating ability. It plays a crucial role in preparing the root canal system for obturation by removing debris, smear layers, and promoting improved adhesion of sealers and irrigants.
Table of Contents
ToggleChemical Properties of EDTA
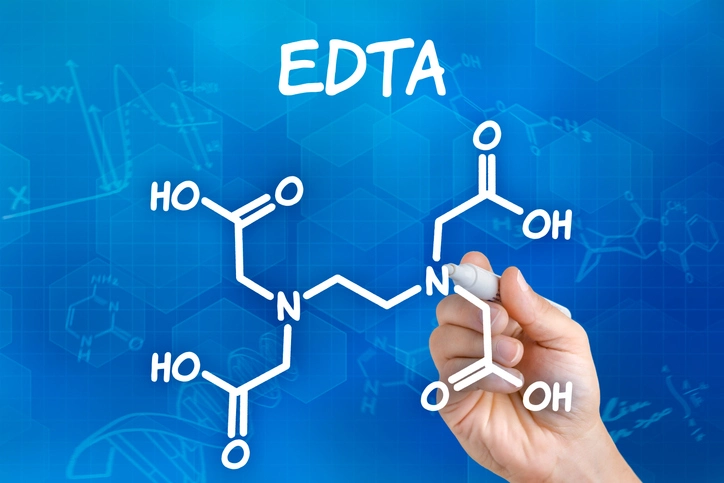
EDTA, or ethylenediaminetetraacetic acid, is a synthetic compound classified as a polyamino carboxylic acid. It is one of the most powerful and widely used chelating agents in both medical and industrial fields due to its strong ability to form complexes with metal ions. Understanding the chemical nature of EDTA is crucial to appreciating its role in dental applications, especially in root canal therapy and dentin conditioning.
Molecular Structure
The molecular formula of EDTA is C₁₀H₁₆N₂O₈, with a molecular weight of approximately 292.24 g/mol. Structurally, EDTA consists of:
- Two nitrogen atoms (from the ethylenediamine component)
- Four acetic acid groups (each containing a carboxyl group, –COOH)
- A central ethylene (–CH₂–CH₂–) backbone connecting the nitrogen atoms
These functional groups give EDTA a total of six potential binding sites, making it a hexadentate ligand. Each EDTA molecule can form six coordinate bonds with a metal ion, effectively encapsulating the ion in a highly stable, water-soluble complex.
Chelation Mechanism
The term chelation comes from the Greek word chele, meaning “claw,” which appropriately describes how EDTA binds to metal ions. Each EDTA molecule “claws” onto a metal ion such as calcium (Ca²⁺), magnesium (Mg²⁺), iron (Fe³⁺), or zinc (Zn²⁺), forming a ring-like structure known as a chelate complex.
In the context of dentistry, EDTA is primarily used to chelate calcium ions in hydroxyapatite (Ca₁₀(PO₄)₆(OH)₂), the major mineral component of dentin and enamel. This action results in:
- Decalcification of the dentin surface
- Opening of dentinal tubules
- Softening of the dentin matrix
This chelating action facilitates both the mechanical shaping of the root canal and the removal of the smear layer.
Acid-Base Behavior and pH
EDTA is a weak polyprotic acid, meaning it has multiple dissociable protons. It exhibits complex acid-base behavior, undergoing stepwise deprotonation of its four carboxylic acid groups and two amine groups depending on the pH of the solution:
- pKa₁ ≈ 0.0
- pKa₂ ≈ 1.5
- pKa₃ ≈ 2.0
- pKa₄ ≈ 2.66
- pKa₅ ≈ 6.13
- pKa₆ ≈ 10.37
At neutral to mildly alkaline pH (~7–8), as is typical for dental use, EDTA exists primarily in its fully or nearly fully deprotonated anionic form, which enhances its affinity for metal cations.
In dentistry, EDTA is commonly used in a 17% aqueous solution with a pH close to 7.0. The neutral pH maintains a balance between effective chelation and biocompatibility, minimizing the risk of tissue irritation when applied inside the root canal.
Solubility and Stability
EDTA is highly soluble in water, especially in its salt forms such as:
- Disodium EDTA (Na₂EDTA) – used in many dental applications
- Tetrasodium EDTA (Na₄EDTA) – used in formulations requiring higher pH
- Calcium disodium EDTA – used in medicine for heavy metal detoxification
The disodium salt of EDTA is most commonly used in dentistry due to its ideal balance between solubility, pH, and chelating power.
In aqueous solution, EDTA is chemically stable over a wide pH range (2–10), although its chelation efficiency decreases in very acidic or highly basic environments. It is also stable under most storage conditions but should be protected from microbial contamination in solution form.
Thermodynamic Stability of Metal Complexes
EDTA forms very stable complexes with metal ions. The formation constant (log Kf) of EDTA-metal complexes is high, indicating a strong and irreversible binding:
- Ca²⁺: log Kf ≈ 10.7
- Mg²⁺: log Kf ≈ 8.7
- Fe³⁺: log Kf ≈ 25.1
- Zn²⁺: log Kf ≈ 16.5
These high constants make EDTA an effective agent for removing calcium ions from hydroxyapatite in dentin, as well as for detoxifying metals in other medical or industrial applications.
EDTA Derivatives and Modifications
Several chemical modifications of EDTA have been developed to improve specificity, reduce toxicity, or modify pH:
- EDTA mono- and diesters: Used in less polar solvents
- EDTA-diamides: Offer selective chelation for specific metal ions
- EDTA conjugates: Coupled with antimicrobial agents, surfactants, or drugs to combine chelation with bioactivity
These derivatives are of emerging interest in advanced dental materials, nanomedicine, and targeted drug delivery systems.
Summary of Chemical Properties
| Property | Description |
|---|---|
| Molecular Formula | C₁₀H₁₆N₂O₈ |
| Molar Mass | ~292.24 g/mol |
| Number of Binding Sites | 6 (hexadentate) |
| pH of Common Formulations | Neutral (around 7.0) |
| Common Dental Form | 17% Na₂EDTA solution |
| Chelation Targets | Primarily Ca²⁺ (also Fe³⁺, Mg²⁺, Zn²⁺) |
| Solubility | High in water (especially as salt) |
| Stability | Thermodynamically stable, especially at pH 6–10 |
Clinical Relevance of These Properties in Dentistry
Understanding EDTA’s chemical properties is more than academic—it is directly tied to its clinical performance:
- The hexadentate chelation explains its efficiency in removing inorganic debris and smear layers.
- Its neutral pH and stability make it safe for intra-canal use.
- High formation constants guarantee strong and irreversible calcium binding, essential for decalcifying dentin.
- Solubility ensures it can be flushed easily and doesn’t obstruct instrumentation or obturation.
In short, these chemical features underpin EDTA’s wide adoption in clinical endodontics and its central role in ensuring successful root canal therapy.
Clinical Applications in Dentistry
The clinical significance of EDTA in dentistry is primarily rooted in its powerful chelating properties, which make it an indispensable agent in modern endodontic therapy. Over the decades, EDTA has transitioned from an auxiliary agent to a central component in root canal cleaning and shaping protocols. Beyond its use in endodontics, it also plays roles in adhesive dentistry and other fields where dentin surface management is critical.
This section delves into the comprehensive clinical applications of EDTA in dentistry, covering both conventional and emerging uses.
Root Canal Irrigation
EDTA is primarily employed in endodontic irrigation protocols to enhance canal debridement. Mechanical instrumentation, whether manual or rotary, leaves behind a smear layer, a byproduct of cutting dentin. This smear layer consists of both organic components (pulp remnants, bacteria, necrotic tissue) and inorganic components (dentin debris, hydroxyapatite crystals).
While sodium hypochlorite (NaOCl) is effective in dissolving organic material, it has minimal effect on the inorganic portion. EDTA, being a calcium chelating agent, is specifically used to remove the inorganic content, effectively eliminating the smear layer and exposing dentinal tubules.
Smear Layer Removal and Tubule Exposure
The removal of the smear layer enhances:
- Irrigant penetration into dentinal tubules
- Antimicrobial effectiveness
- Adhesion of root canal sealers and restorative materials
- Long-term sealability of the canal system
Scanning Electron Microscopy (SEM) studies have consistently shown that a 17% EDTA solution, applied for 1–5 minutes, is effective in completely removing smear layers from the coronal and middle thirds of the root canal, though its efficacy in the apical third is somewhat reduced due to limited irrigant penetration.
Lubrication and Debris Removal During Instrumentation
EDTA is frequently included in gel-based lubricants used during mechanical instrumentation. These preparations (e.g., RC-Prep, File-Eze) serve multiple purposes:
- Reduce friction between the file and canal walls
- Facilitate easier file advancement, particularly in curved or narrow canals
- Trap and suspend debris, helping prevent blockage or canal transportation
- Minimize instrument separation due to smoother motion
These products typically combine EDTA with a mild oxidizer like urea peroxide or surfactants that further enhance cleansing action and visibility through mild effervescence.
Apical Patency and Management of Calcified Canals
One of the more challenging aspects of endodontic therapy is negotiating calcified or sclerosed canals, particularly in older patients or following trauma. In such cases, EDTA is used to:
- Softening dentin obstructions by chelating calcium
- Facilitate reestablishment of canal patency
- Prevent iatrogenic errors, such as ledging, zipping, or transportation
EDTA gels, when left inside a calcified canal for several minutes, can soften mineral deposits enough to allow the reintroduction of small files (e.g., #08 or #10 K-files), often with the assistance of ultrasonic activation or precurved instruments.
Enhancing Adhesion of Sealers and Restorative Materials
By removing the smear layer and exposing the underlying collagen matrix and dentinal tubules, EDTA improves the micromechanical adhesion of:
- Resin-based sealers (e.g., AH Plus, Epoxy resin-based sealers)
- Bonding agents for post cementation
- Adhesive restorations (in coronal dentin preparation)
This is especially relevant in procedures such as post and core placement, where optimal bond strength to root dentin is crucial. A properly conditioned canal wall ensures deeper resin tag formation, which improves retention and reduces microleakage.
Use in Regenerative Endodontics
In regenerative endodontics, particularly with immature permanent teeth undergoing revascularization procedures, EDTA plays a unique role. Unlike NaOCl, which is cytotoxic to stem cells, EDTA is:
- Biocompatible with apical stem cells
- Capable of exposing dentin-derived growth factors like TGF-β, which promote cellular proliferation and differentiation
- Used in the final rinse to create a favorable microenvironment for tissue ingrowth
For this reason, protocols recommended by the American Association of Endodontists (AAE) often advocate a final rinse with 17% EDTA in regenerative procedures to encourage stem cell migration and attachment.
Role in Retreatment Cases
In endodontic retreatment cases, where canals are already obturated, EDTA is used in combination with solvents and mechanical instrumentation to:
- Aid in gutta-percha removal
- Help dissolve root canal sealers, particularly those containing zinc oxide
- Remove residual filling materials from lateral and accessory canals
- Recondition canal walls for effective resealing
Its ability to chelate and soften residual filling material facilitates more complete debridement in these often-complex cases.
Periodontics and EDTA Use
Though less common than in endodontics, EDTA has also found occasional use in periodontics, specifically in procedures like:
- Root surface conditioning prior to guided tissue regeneration (GTR)
- Demineralization of root surfaces to expose collagen fibers, theoretically improving the attachment of connective tissue and cells
However, its efficacy in periodontal regeneration remains debated, and its use in this context is not routine.
Pediatric Endodontics
In pediatric dentistry, where primary teeth often present with narrow or tortuous canals, EDTA can:
- Facilitate instrumentation by softening dentin
- Improve cleaning in hard-to-reach areas
- Be safely used when avoiding apical extrusion due to its relatively lower toxicity compared to NaOCl
Some pediatric practitioners use a reduced concentration (e.g., 10% EDTA) in children to further minimize any risk of periapical irritation.
Use with Ultrasonic and Laser Activation
Recent advances in irrigant activation techniques have further improved the effectiveness of EDTA. These include:
- Passive ultrasonic irrigation (PUI): Enhances the penetration of EDTA into canal irregularities and dentinal tubules.
- Laser-activated irrigation (LAI): Induces cavitation and acoustic streaming to improve EDTA effectiveness.
- Sonic irrigation systems (e.g., EndoActivator): Facilitate EDTA circulation and increase contact with canal walls.
These technologies expand the clinical effectiveness of EDTA by ensuring better distribution, surface contact, and cleaning efficacy, especially in complex canal anatomies like isthmuses, lateral canals, and apical deltas.
Summary of Clinical Applications
| Application | Purpose |
|---|---|
| Root canal irrigation | Smear layer removal, dentin conditioning |
| Instrumentation lubrication | Reduce friction, enhance debris removal |
| Calcified canal management | Softens calcified tissue to enable negotiation |
| Enhancing adhesion | Improves bonding of sealers and posts |
| Regenerative endodontics | Releases growth factors, supports stem cell survival |
| Retreatment | Assists in removal of obturation materials |
| Periodontics (adjunctive) | Root surface conditioning for potential tissue reattachment |
| Pediatric endodontics | Safe dentin softening and smear layer removal in primary teeth |
| Irrigant activation systems | Improves penetration and effectiveness in complex canal anatomies |
Application Protocols and Techniques
The clinical success of endodontic procedures depends not only on the selection of irrigants but also on how they are applied. The use of EDTA (ethylenediaminetetraacetic acid) requires precise protocols that optimize its chelating efficiency while minimizing potential adverse effects like dentin erosion or chemical incompatibilities.
EDTA is typically used in a 17% concentration in either solution or gel form, and its application is timed and sequenced to work synergistically with other agents like sodium hypochlorite (NaOCl). Proper implementation involves understanding when, how much, how long, and in what sequence to use EDTA in clinical scenarios.
Typical Irrigation Sequence in Root Canal Therapy
An effective irrigation protocol involving EDTA typically follows this multi-step sequence:
Initial irrigation with NaOCl (2.5%–5.25%)
Purpose: Dissolution of organic tissue and antimicrobial action.
Used throughout instrumentation to disinfect and lubricate.
Intermittent irrigation with EDTA (17%)
Purpose: Smear layer removal, dentin conditioning.
Applied after canal shaping is complete or between file sizes to prevent smear accumulation.
Final rinse with EDTA (17%)
Purpose: Complete smear layer removal and exposure of dentinal tubules to improve sealer adhesion.
Optional final rinse with NaOCl
Purpose: Disinfection of opened dentinal tubules, further organic tissue dissolution.
Applied for a short duration (30 seconds to 1 minute) after EDTA to avoid over-erosion.
Duration of Application
Time of exposure is a critical factor influencing the effectiveness and safety of EDTA. Excessive exposure can lead to erosion of peritubular and intertubular dentin, weakening the tooth structure.
| Application Site | Recommended Exposure Time |
|---|---|
| Coronal third | 1–2 minutes |
| Middle third | 1–2 minutes |
| Apical third | 30 seconds – 1 minute |
Clinical studies recommend a total contact time of 1–3 minutes, especially in the final irrigation step, to achieve optimal smear layer removal without inducing dentinal erosion.
Volume of EDTA Used
The volume of EDTA delivered into the canal can vary depending on the canal length and complexity, but typical volumes range from 3 to 10 mL per canal.
- Minimalist approaches use 2–3 mL of EDTA as a final rinse.
- More aggressive debridement protocols may use up to 10 mL for thorough irrigation and activation, especially in large or complex canals.
Delivery Techniques
Conventional Syringe Irrigation
The most commonly used technique involves:
- A 30-gauge side-vented needle
- Inserted 1–2 mm short of the working length
- Gentle, controlled irrigation to prevent apical extrusion
Advantages:
- Widely available and cost-effective
- Easy to perform
Limitations:
- Limited irrigant penetration into lateral canals or apical third
- May not adequately clean canal irregularities
Agitation and Activation Techniques
To enhance the penetration and efficacy of EDTA, especially in the apical third and lateral anatomies, several activation methods are used:
a) Passive Ultrasonic Irrigation (PUI)
- Involves placing an ultrasonic file or tip into the canal filled with EDTA.
- Ultrasonic energy creates acoustic streaming and cavitation, enhancing smear layer removal.
b) Sonic Activation (e.g., EndoActivator)
- Generates high-frequency oscillations that agitate the irrigant within the canal.
- Improves contact with canal walls and penetration into accessory canals.
c) Negative Pressure Systems (e.g., EndoVac)
- Delivers EDTA to the apical third using negative pressure to draw the solution downward.
- Reduces risk of extrusion and ensures deeper irrigant delivery.
d) Laser-Activated Irrigation (LAI)
- EDTA is agitated using Er:YAG or diode lasers to generate shockwaves in the canal.
- Provides superior smear layer removal in some studies.
e) Manual Dynamic Agitation (MDA)
- Involves moving a well-fitted gutta-percha cone up and down in the canal filled with EDTA.
- Increases wall contact without requiring advanced equipment.
Gel vs. Liquid Formulations
EDTA is available in both gel and liquid formulations, each with distinct clinical indications:
| Formulation | Advantages | Common Uses |
|---|---|---|
| Liquid (17%) | Easy to flush, covers entire canal | Final rinse, smear layer removal |
| Gel/Paste (e.g., RC-Prep) | Provides lubrication, localized action | During filing, negotiation of calcified canals |
Combination protocols may use gel EDTA during instrumentation followed by liquid EDTA during the final rinse.
Application in Specific Clinical Scenarios
Narrow and Calcified Canals
- Use EDTA gel or liquid for pre-treatment to soften dentin.
- Apply for 3–5 minutes with ultrasonic activation.
Retreatment
- Apply EDTA after removing obturation material to soften debris and recondition dentin.
- May help loosen hard-set sealers for easier removal.
Regenerative Endodontics
- Use as a final rinse (17%, 1–2 minutes) after NaOCl to expose growth factors and improve stem cell adhesion.
- Avoid reintroducing NaOCl afterward to preserve the exposed collagen matrix.
Pediatric Endodontics
- Use reduced concentration (e.g., 10–12%) and shorter exposure times to minimize irritation.
- Apply passively with a side-vented needle, especially in primary teeth.
Post-EDTA Protocol Considerations
After the use of EDTA, clinicians must consider the potential interaction with residual NaOCl or chlorhexidine:
- Avoid mixing EDTA directly with CHX: This can produce a white precipitate (parachloroaniline), potentially cytotoxic.
- Use sterile saline or distilled water between irrigants to avoid interactions.
Innovations and Protocol Optimization
Recent research focuses on improving the delivery and efficacy of EDTA through:
- Chelator cocktails combining EDTA with surfactants or antibacterials
- Controlled-release EDTA formulations embedded in endodontic gels
- Nanoparticle-assisted chelation, where EDTA is attached to silver or calcium-based nanoparticles for dual antimicrobial and smear-removal action
- EDTA-loaded gutta-percha cones for slow, sustained dentin conditioning in complex cases
Interaction with Other Irrigants
Endodontic irrigation relies on a multi-agent approach, since no single solution is capable of achieving all the goals of root canal disinfection, lubrication, smear layer removal, and tissue dissolution. EDTA (Ethylenediaminetetraacetic acid) is a critical part of this irrigation strategy, but its effectiveness—and safety—depend heavily on how it interacts with other commonly used irrigants.
This section provides an in-depth look at EDTA’s chemical compatibility, sequencing rationale, biological implications, and potential risks when combined or alternated with sodium hypochlorite (NaOCl), chlorhexidine (CHX), citric acid, MTAD, and other agents.
EDTA and Sodium Hypochlorite (NaOCl)
NaOCl Overview
- Concentration: Typically 2.5%–5.25%
- Function: Dissolves organic tissues, kills microbes, disrupts biofilms
Synergistic Use
EDTA and NaOCl are the cornerstones of modern irrigation protocols. Each targets different components:
- NaOCl: Organic matter (pulp, collagen, biofilm)
- EDTA: Inorganic matter (hydroxyapatite, smear layer)
When used sequentially, they provide complementary actions:
- NaOCl dissolves organic debris.
- EDTA removes the inorganic smear layer, exposing dentinal tubules.
- A final rinse with NaOCl disinfects the newly exposed tubules and flushes out residues.
Cautions and Limitations
Direct mixing of NaOCl and EDTA results in chemical neutralization.
EDTA reduces the available chlorine in NaOCl, compromising its antimicrobial efficacy.
A visible color change (from clear to brownish) indicates chlorine loss.
Avoid storing them in the same syringe or chamber.
Always rinse with saline or distilled water between irrigants to prevent neutralization.
Effect on Dentin
Extended use of EDTA followed by NaOCl can cause dentin erosion and loss of microhardness.
To minimize this:
Use EDTA for no more than 1–3 minutes.
Follow with a brief NaOCl rinse (30 seconds–1 minute).
EDTA and Chlorhexidine (CHX)
CHX Overview
- Concentration: 0.2%–2.0%
- Function: Broad-spectrum antimicrobial; high substantivity
- Limitation: Cannot dissolve tissue or remove smear layer
Potential Precipitate Formation
When EDTA is mixed with CHX, a white-to-brown precipitate forms, often referred to as parachloroaniline (PCA). This has several clinical concerns:
- Cytotoxicity: PCA has potential toxic and carcinogenic effects.
- Tubule blockage: The precipitate may occlude dentinal tubules, compromising sealer penetration.
- Unpredictable outcomes: Formation depends on concentration, pH, and sequence.
Clinical Recommendations
Never use CHX immediately after EDTA without an intermediate rinse (preferably saline or distilled water).
To use CHX safely:
- Irrigate with NaOCl.
- Use EDTA for smear removal.
- Rinse thoroughly with saline.
- Apply CHX as the final rinse (optional).
EDTA and Citric Acid
Citric Acid Overview
- Concentration: Usually 10%–50%
- Function: Organic acid with chelating properties, similar to EDTA
Comparison to EDTA
Both EDTA and citric acid effectively remove the smear layer.
Citric acid has a lower pH (~1.0–2.5), which can:
Cause greater dentin demineralization
Lead to tissue irritation if extruded
EDTA is generally preferred due to:
Neutral pH (~7.0)
Less aggressive decalcification
Better biocompatibility
Compatibility
Citric acid and EDTA are not used together but may be considered interchangeable in certain protocols. For patients with sensitivities or for use in regenerative procedures, citric acid may offer advantages in controlled applications.
EDTA and MTAD
MTAD Overview
Components:
Doxycycline (3%) – broad-spectrum antibiotic
Citric acid (4.25%) – smear layer remover
Tween 80 (0.5%) – detergent/surfactant
Function: Combines antimicrobial activity with smear removal
EDTA as Pre-treatment
Many protocols suggest using EDTA before MTAD to:
- Prime the canal by removing the smear layer
- Allow deeper penetration of doxycycline into tubules
However, using both EDTA and MTAD together may exacerbate dentin erosion, particularly in the apical third.
Clinical Tips
If using MTAD:
Consider replacing EDTA with MTAD as the final rinse.
Do not use EDTA and MTAD in immediate succession without evaluating the risk of over-decalcification.
EDTA and QMiX
QMiX Overview
A combination of:
- CHX (antibacterial)
- EDTA (chelator)
- Detergents
Advantages
- Offers smear layer removal and antimicrobial action in a single irrigant.
- Designed to be used as a final rinse after NaOCl.
Compatibility
QMiX avoids the precipitate formation issues seen when CHX and EDTA are used separately. However, it should not be mixed with NaOCl, as it can still result in chlorine gas or PCA-like precipitates.
Clinical Protocol
- Use NaOCl for bulk debridement.
- Rinse thoroughly with saline.
- Apply QMiX as the final irrigant.
Summary Table of EDTA Interactions
| Irrigant | Purpose | Interaction with EDTA | Clinical Recommendation |
|---|---|---|---|
| NaOCl | Dissolves organic tissue, disinfection | Neutralizes if mixed directly | Use sequentially; rinse between |
| CHX | Antimicrobial with substantivity | Forms precipitate (PCA) | Rinse between with saline; avoid direct mix |
| Citric Acid | Chelator (acidic) | Similar function; more aggressive decalcification | Use one or the other; EDTA preferred |
| MTAD | Antibiotic + chelator + detergent | Redundant smear removal | Use one; avoid both to prevent erosion |
| QMiX | EDTA + CHX combo | Designed to avoid PCA | Rinse NaOCl thoroughly before use |
Intermediate Rinsing
Between irrigants, especially those with known chemical incompatibilities, the use of an intermediate rinse is essential. Recommended intermediate irrigants:
- Sterile saline
- Distilled water
- Alcohol rinse (in some protocols, to dry canal)
This simple step can prevent precipitate formation, maintain irrigant efficacy, and reduce cytotoxicity.
Advantages of EDTA in Dentistry
EDTA (Ethylenediaminetetraacetic acid) is considered one of the most important auxiliary agents in contemporary dentistry, particularly in endodontic therapy. Its advantages stem from its unique chelating ability, biocompatibility, and its ability to enhance the efficacy of other irrigants and restore the structural and biological integrity of dentin.
This section highlights the broad spectrum of advantages that EDTA offers in dental applications, particularly in endodontics, restorative procedures, and regenerative approaches.
Effective Smear Layer Removal
The primary and most well-documented advantage of EDTA is its ability to remove the smear layer generated during mechanical instrumentation of the root canal system.
Why It Matters:
The smear layer acts as a physical barrier that blocks antimicrobial agents and sealers from penetrating the dentinal tubules.
Removal of this layer is essential for:
Improved canal disinfection
Better adhesion of root filling materials
Prevention of bacterial recontamination
How EDTA Helps:
- EDTA chelates calcium ions in hydroxyapatite, dissolving the inorganic component of the smear layer.
- When used after sodium hypochlorite (which removes the organic portion), EDTA ensures complete smear removal, enhancing the thoroughness of canal cleaning.
Opens Dentinal Tubules for Irrigant and Sealer Penetration
Following the removal of the smear layer, EDTA opens dentinal tubules, allowing for:
Deeper penetration of irrigants, such as chlorhexidine or NaOCl, into the canal walls.
Greater infiltration of sealers and adhesives, which leads to:
Stronger micromechanical retention
Reduced microleakage
Improved long-term sealing of the canal system
This is particularly important in obturation, as open tubules enhance the adaptation and entombment of residual bacteria, reducing the risk of failure.
Facilitates Instrumentation in Narrow or Calcified Canals
In complex cases involving sclerotic, calcified, or narrow canals, EDTA plays a key role in softening dentin and facilitating instrumentation.
Clinical Benefits:
- Reduces the risk of procedural errors such as ledging, transportation, or instrument separation.
- Improves the clinician’s ability to negotiate curved or constricted canals.
- Enhances the action of hand and rotary files, particularly in older patients or teeth with trauma-induced calcification.
Enhances Adhesion of Root Canal Sealers and Restorative Materials
EDTA is frequently used to condition dentin prior to:
- Post and core placement
- Resin-bonded restorations
- Fiber post cementation
By removing smear layers and exposing the collagen matrix and intertubular dentin, EDTA improves adhesive bonding. This enhances:
- Retention strength
- Marginal integrity
- Longevity of restorations
This benefit is significant in both coronal restoration and intraradicular post systems where bonding to dentin is critical.
Biocompatibility and Safety (When Used Appropriately)
Compared to stronger acids (e.g., phosphoric acid or citric acid), EDTA has a neutral to slightly alkaline pH (7.0–8.0), making it:
- Less cytotoxic when extruded beyond the apex
- Gentler on periapical tissues
- Safe for use in immature teeth or regenerative procedures
This low irritant profile makes EDTA particularly suitable for use in:
- Pediatric patients
- Regenerative endodontics
- Cases with open apices or thin canal walls
Synergistic Use with Other Irrigants
EDTA enhances the overall efficacy of other irrigants by:
- Following sodium hypochlorite to remove the inorganic smear component
- Preconditioning dentin to improve the uptake and action of chlorhexidine or antibiotics (e.g., MTAD)
- Allowing disinfectants to reach deeper layers, thanks to improved dentin permeability
When used correctly (with proper intermediate rinses), EDTA enables a layered chemical approach to root canal disinfection.
Versatility in Form and Application
EDTA is available in multiple formulations, making it adaptable to various clinical needs:
| Form | Common Use | Advantages |
|---|---|---|
| Liquid (17%) | Final irrigation | Deep penetration, ease of flushing |
| Gel (e.g., RC-Prep) | During instrumentation | Lubrication, safer in curved/narrow canals |
| Paste | Retreatment, calcified canals | Localized effect, controlled application |
This versatility ensures that EDTA can be integrated at multiple stages of treatment, tailored to the clinician’s workflow and the specific anatomy of the canal system.
Promotes Growth Factor Release in Regenerative Procedures
EDTA has been shown to release biologically active growth factors (e.g., TGF-β, VEGF) from dentin when used as a final irrigant in regenerative endodontic procedures.
Implications:
- Stimulates stem cell adhesion, migration, and differentiation
- Promotes angiogenesis and tissue repair
- Encourages the formation of new dentin-like tissue
For these reasons, EDTA is strongly recommended in protocols for:
- Revascularization
- Apexogenesis
- Immature teeth with necrotic pulps
Cost-Effective and Readily Available
EDTA is an inexpensive, shelf-stable agent that is:
- Easily incorporated into routine dental practice
- Compatible with most endodontic systems
- Widely supported by decades of clinical use and research
Given its broad utility, its cost-to-benefit ratio makes it one of the most valuable adjuncts in endodontic treatment.
Evidence-Based Support
Numerous in vitro, in vivo, and clinical studies support the use of EDTA. Highlights include:
- SEM imaging proving its smear layer removal ability
- Studies showing increased bond strength when EDTA precedes adhesive applications
- Research indicating enhanced antimicrobial penetration when canals are conditioned with EDTA
- Systematic reviews validating its role in improving root canal sealability
The evidence-based foundation for EDTA use gives clinicians confidence in its effectiveness and predictability.
Limitations and Drawbacks
While EDTA (ethylenediaminetetraacetic acid) offers numerous advantages in dental practice—particularly in endodontics—its use is not without limitations. Like any chemical adjunct, improper use, overuse, or misunderstanding of its properties can result in complications that compromise clinical outcomes.
This section explores the chemical, biological, mechanical, and clinical limitations associated with EDTA, including known risks, controversies, and the practical considerations that dental professionals must be aware of.
Lack of Antimicrobial Activity
Primary Limitation:
EDTA does not possess strong antimicrobial properties, particularly against common endodontic pathogens such as Enterococcus faecalis, Candida albicans, or anaerobic bacteria found in biofilms.
Clinical Implication:
- Cannot be used as a stand-alone irrigant for disinfection
- Ineffective in killing bacteria, particularly in the deeper layers of dentinal tubules
- Requires combination with sodium hypochlorite (NaOCl) or chlorhexidine (CHX) to achieve full-spectrum antimicrobial efficacy
Mitigation:
- Use EDTA as part of a sequential irrigation protocol
- Always pair it with a disinfecting agent for effective canal sterilization
Potential for Dentinal Erosion
Mechanism:
Extended exposure of dentin to EDTA can result in chelation of calcium from both the smear layer and the underlying dentin, leading to:
- Demineralization
- Structural weakening
- Erosion of peritubular and intertubular dentin
Clinical Manifestation:
- Softening of dentin, especially in the apical third
- Loss of microhardness, which may impair the tooth’s resistance to fracture
- Increased dentin permeability, which can inadvertently enhance leakage if not properly sealed
Evidence:
Studies using Scanning Electron Microscopy (SEM) and microhardness testing have confirmed that EDTA can cause surface deterioration when used for more than 1–3 minutes or in large volumes.
Mitigation:
- Limit EDTA exposure to 1–2 minutes per canal segment
- Avoid prolonged soaking or leaving EDTA in the canal
- Follow EDTA use with thorough flushing and careful obturation
Interaction with Other Irrigants
Risks of Chemical Incompatibility:
EDTA can interact negatively with several commonly used irrigants:
- NaOCl: EDTA neutralizes the chlorine in sodium hypochlorite, reducing its antimicrobial and tissue-dissolving abilities
- CHX: Direct mixing with chlorhexidine produces a white-to-brown precipitate (parachloroaniline), which is potentially cytotoxic and carcinogenic
Clinical Impact:
- Inactivation of key irrigants
- Formation of harmful by-products
- Blockage of dentinal tubules, reducing the effectiveness of subsequent sealing
Mitigation:
- Use saline or distilled water rinses between irrigants
- Avoid direct mixing or simultaneous delivery of incompatible solutions
- Educate staff on correct irrigation sequences
Limited Penetration in Complex Anatomy
While EDTA effectively removes the smear layer from straight canals, it has limited penetration in:
- Isthmuses
- Lateral canals
- Apical deltas
- Curved or S-shaped roots
Contributing Factors:
- Inadequate delivery method (e.g., syringe only)
- Lack of activation (ultrasonic, sonic, or negative pressure)
Clinical Implication:
- Residual debris and smear in untouched areas may persist
- Incomplete conditioning of dentin may compromise disinfection and obturation
Mitigation:
- Use irrigant activation systems (e.g., Passive Ultrasonic Irrigation, EndoActivator, EndoVac)
- Use side-vented needles and place as close as possible to working length without extruding
No Effect on Organic Components
EDTA is designed to remove inorganic material. It is incapable of dissolving or disrupting:
- Pulpal remnants
- Organic debris
- Necrotic tissue
- Bacterial biofilms
This limitation further reinforces its dependence on NaOCl or other tissue solvents to perform complete canal cleaning.
Potential for Apical Extrusion and Periapical Irritation
Though generally less cytotoxic than NaOCl, extrusion of EDTA beyond the apical foramen can still lead to:
- Periapical inflammation
- Pain or swelling
- Delayed healing, especially in cases with open apices or immature teeth
Mitigation:
- Use side-vented irrigation needles
- Do not force irrigants into the canal; apply with gentle pressure
- Terminate needle tip 1–2 mm short of working length
- Use gel formulations in high-risk cases for safer application
Limited Shelf-Life and Storage Considerations
While EDTA is generally stable, certain commercial formulations may:
- Be sensitive to light or heat
- Undergo microbial contamination if not stored properly
- Lose efficacy when contaminated with other irrigants
Mitigation:
- Store in cool, dark places
- Follow manufacturer’s expiration dates
- Use fresh solution when possible
Risk of Overuse in Retreatment and Regenerative Cases
In retreatment cases or regenerative endodontics, repeated or excessive use of EDTA can:
- Over-demineralize dentin
- Interfere with growth factor release timing
- Compromise stem cell viability in the root canal space
Mitigation:
- Tailor EDTA exposure time to clinical goals (1–2 minutes max in regenerative cases)
- Avoid redundant use during re-entry unless clearly needed
- Combine with biocompatible sealing protocols
Environmental and Waste Management Concerns
As a synthetic chelating agent, EDTA is:
- Non-biodegradable
- Persistent in wastewater systems
- Capable of binding heavy metals in the environment, possibly altering ecosystems
Mitigation:
- Minimize unnecessary use
- Dispose of EDTA-containing waste according to local environmental regulations
- Explore biodegradable alternatives (e.g., phytic acid, chitosan) where possible
Summary of Limitations and Clinical Considerations
| Limitation | Clinical Risk | Best Practice |
|---|---|---|
| Lack of antimicrobial action | Incomplete disinfection | Always pair with NaOCl or CHX |
| Dentin erosion | Weakened canal walls | Limit exposure to ≤3 minutes |
| Incompatibility with other irrigants | Precipitate formation, chemical inactivation | Use intermediate saline rinses between solutions |
| Limited access to complex anatomy | Incomplete smear removal | Use irrigation activation techniques |
| No effect on organic debris | Retained pulp tissue | Use NaOCl first for organic dissolution |
| Potential for apical extrusion | Periapical inflammation | Use side-vented needles, gentle irrigation |
| Overuse in special cases | Erosion or healing interference | Adjust protocol for retreatment or regeneration |
| Environmental concerns | Waste accumulation in ecosystems | Dispose responsibly, consider biodegradable options |
EDTA Formulations in Dentistry
The clinical effectiveness of EDTA (ethylenediaminetetraacetic acid) in dentistry is not only a result of its chemical properties but also of its formulation, which determines how it is delivered, how it interacts with tissues and other agents, and how safely it can be used within the canal system. Over the years, dental manufacturers have developed various EDTA-based products tailored to specific clinical scenarios, offering different viscosities, additives, pH levels, and delivery mechanisms.
This section explores the key types of EDTA formulations used in dental practice, particularly endodontics, including liquid, gel, and paste forms, along with examples, indications, and clinical considerations.
Types of EDTA Formulations
EDTA is available in several formulations:
| Formulation Type | Typical Concentration | Primary Use |
|---|---|---|
| Liquid | 17% | Final irrigation, smear layer removal |
| Gel | ~15–17% | Instrumentation lubrication, calcified canals |
| Paste | ~10–17% | Localized application, heavily calcified or retreatment cases |
Each of these forms may be standalone EDTA or combined with additional agents such as surfactants, peroxides, or antimicrobials to enhance performance.
Liquid EDTA Formulations
Liquid EDTA solutions are the most common and widely used formulation. They are typically 17% aqueous solutions of disodium EDTA with a pH of around 7.0–8.0, designed to be used as final irrigants for smear layer removal.
Commercial Examples:
SmearClear® (SybronEndo)
17% EDTA solution with added surfactants for enhanced wettability
Increases penetration into dentinal tubules and improves flow
Vista-EDTA™ (Vista Dental)
A clear solution with high purity and consistent pH control
EDTA Solution (Pulpdent)
Standard 17% EDTA used as a final rinse
Advantages:
- Easy to deliver using syringes or irrigation systems
- Ideal for use with irrigant activation technologies (ultrasonic, sonic, laser)
- Covers the entire canal length efficiently
Limitations:
- Higher risk of apical extrusion if not carefully delivered
- Rapid flow may reduce contact time in some anatomical areas
Best Use:
- As a final irrigant after NaOCl
- When used with agitation systems for enhanced penetration
- In regenerative procedures to expose dentin-derived growth factors
Gel-Based EDTA Formulations
Gel-based formulations of EDTA are viscous, often transparent or opaque, and contain approximately 15–17% EDTA combined with lubricants, surfactants, or effervescent agents.
Commercial Examples:
RC-Prep® (Premier Dental)
Contains 15% EDTA and 10% urea peroxide
Generates mild effervescence during instrumentation to lift debris
File-Eze® (Ultradent)
Contains EDTA and CMC (carboxymethylcellulose) for viscosity
Includes lubricants and antimicrobials
Glyde® File Prep (Dentsply Sirona)
A gel containing EDTA, hydrogen peroxide, and a surfactant
Known for bubble formation, aiding in debris removal
Advantages:
- Reduces friction between instruments and dentin
- Improves debris removal by acting as a suspension medium
- Minimizes apical extrusion due to controlled viscosity
- Easier length control during hand instrumentation
Limitations:
- Not as effective as liquid EDTA for complete smear layer removal
- May require a subsequent rinse with liquid EDTA to clean canal walls thoroughly
- Can clog irrigation needles if not properly flushed
Best Use:
During mechanical instrumentation, especially in:
Curved canals
Narrow or calcified canals
When using manual files, especially stainless steel K-files
Paste EDTA Formulations
Paste formulations are less common but useful in specific applications, especially where localized chelation is required.
Clinical Examples:
- Used in calcified canals where pre-softening is needed
- Applied with microbrushes or carriers into stubborn canal obstructions
Advantages:
- Stays in place for prolonged contact time
- Offers localized demineralization with minimal diffusion
- Useful in retreatment or re-entry of calcified cases
Limitations:
- More difficult to remove completely without thorough irrigation
- Not suitable for general irrigation due to lack of flow
Best Use:
- In calcified or blocked canals where selective softening is needed
- As a spot treatment during re-negotiation
EDTA in Combination Irrigants and Advanced Formulations
Multifunctional Products:
Some newer irrigation products combine EDTA with other agents to simplify protocols:
| Product | Key Ingredients | Function |
|---|---|---|
| QMiX (Dentsply) | EDTA + CHX + surfactant | Final irrigant with smear layer removal and antimicrobial action |
| SmearOFF™ (Vista Dental) | EDTA + CHX derivative + detergent | Dual-action rinse designed to eliminate precipitate risks |
| MTAD (Dentsply) | Citric acid + doxycycline + detergent | An alternative to EDTA with antimicrobial properties |
| BioPure® MTAD | Similar to MTAD | Targets resistant pathogens like E. faecalis |
Advantages:
- Simplify irrigation by combining multiple actions in one solution
- Reduce chair time and potential chemical interaction risks
Limitations:
- Higher cost
- Require careful protocol adherence to avoid reduced efficacy
- Potential for dentin erosion with prolonged exposure
Factors Influencing Product Selection
Clinicians should base their choice of EDTA formulation on several factors:
| Clinical Factor | Recommended Formulation |
|---|---|
| Routine final rinse | Liquid EDTA (17%) |
| Curved/narrow canals | Gel EDTA (e.g., RC-Prep) |
| Calcified canals | Paste or gel formulation |
| Regenerative cases | Pure liquid EDTA without additives |
| Retreatment | Gel with peroxide for effervescence |
| Ultrasonic activation | Liquid EDTA for better flow |
Conclusion
EDTA has cemented its role in modern endodontics as a cornerstone chelating agent. Its ability to effectively remove the smear layer, condition dentin, and facilitate adhesion makes it indispensable. However, its limitations—particularly regarding erosion and lack of antimicrobial properties—necessitate judicious use and integration with complementary agents.
As dental science advances, continued research into improving the efficacy and safety profile of EDTA and its alternatives will drive the evolution of minimally invasive, biologically respectful endodontic treatment protocols. Dentists must remain informed about best practices in EDTA use to ensure optimal outcomes and patient safety.