Sensitive dentin, often referred to as dentin hypersensitivity, is a common dental condition that causes short, sharp pain in response to certain stimuli, such as cold, hot, sweet, or acidic substances, or even physical touch. This condition affects a significant portion of the population and can lead to considerable discomfort and reduced quality of life. Despite its prevalence, the mechanisms, causes, and treatment options for dentin sensitivity are complex and require a nuanced understanding of dental anatomy, physiology, and pathology. In this article, we will explore the structure and function of dentin, the underlying causes and mechanisms of dentin hypersensitivity, and the various treatment approaches available to manage this condition.
Table of Contents
ToggleDentin Structure and Composition
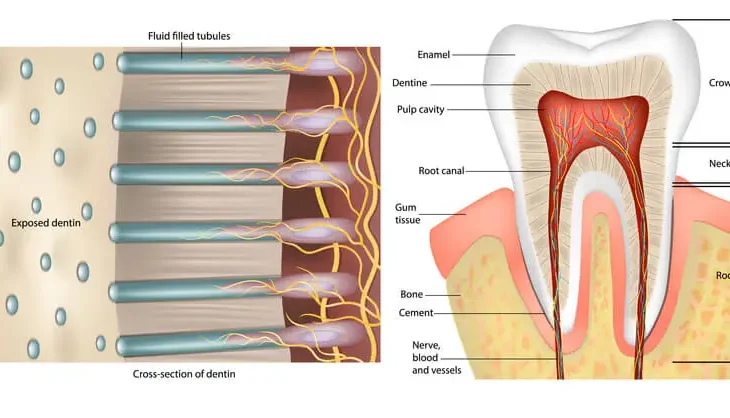
Dentin is a mineralized tissue that forms the bulk of the tooth, lying beneath the enamel in the crown and beneath the cementum in the root. Structurally, dentin consists of microscopic tubules that extend from the outer surface of the tooth (near the enamel-dentin junction or cementum-dentin junction) to the inner pulp chamber. These dentinal tubules play a crucial role in the tooth’s sensory response and are filled with a fluid that can transmit stimuli, ultimately leading to the sensation of pain when exposed.
Dentin’s composition is approximately:
- 70% inorganic material, primarily hydroxyapatite crystals.
- 20% organic matrix, mostly type I collagen and non-collagenous proteins.
- 10% water, contained mainly within the dentinal tubules.
The high mineral content provides structural strength, while the organic component gives dentin some degree of resilience and flexibility, which helps absorb forces during chewing. However, this structure also makes dentin susceptible to sensitivity when the protective enamel or cementum layer is compromised.
Mechanisms of Dentin Hypersensitivity
The pain associated with sensitive dentin is primarily due to the stimulation of the nerves within the dentinal tubules, which communicate with the tooth’s pulp chamber. There are several proposed mechanisms that explain how these nerve endings become stimulated and lead to the sensation of pain. The most widely accepted of these is the hydrodynamic theory.
Hydrodynamic Theory
This theory, proposed by Dr. Martin Brännström in the 1960s, is the most accepted explanation for dentin hypersensitivity. According to the hydrodynamic theory, dentinal hypersensitivity occurs due to the rapid movement of fluid within the dentinal tubules. When external stimuli (e.g., thermal, chemical, or mechanical) are applied to the exposed dentin, they cause the fluid inside the tubules to shift. This movement, in turn, distorts the nerve endings located near the pulp, generating a pain response. Notably:
- Cold stimuli usually induce an outward flow of fluid, leading to sharp pain.
- Heat stimuli cause an inward flow, which also triggers pain but is typically less intense.
Neurogenic Mechanism
Another theory suggests that pain may be directly initiated through the activation of nerve fibers in response to certain stimuli. This neurogenic mechanism is less widely accepted but posits that dentin exposure could lead to an increase in nerve density within the tubules, making them more susceptible to stimulation by external triggers.
Role of Odontoblasts
Odontoblasts, cells located at the interface between the dentin and pulp, may also play a role in dentin hypersensitivity. These cells extend processes into the dentinal tubules and can respond to stimuli, potentially contributing to the sensation of pain. Although this concept is still under investigation, it adds another layer of complexity to our understanding of dentin hypersensitivity.
Causes of Dentin Hypersensitivity
Dentin hypersensitivity arises primarily when the dentinal tubules become exposed to the oral environment. This exposure can occur for several reasons, including the following:
- Gingival Recession and Cementum Loss
- Enamel Erosion and Attrition
- Abfraction Lesions
- Tooth Whitening Procedures
Gingival Recession and Cementum Loss
Gingival recession, often due to periodontal disease or aggressive brushing habits, can lead to the exposure of root dentin. Unlike enamel, which covers the crown of the tooth, cementum is a thin layer that covers the root and provides only minimal protection for the underlying dentin. When this cementum layer is lost, typically through mechanical wear or demineralization, the dentinal tubules are exposed, increasing the likelihood of sensitivity.
Enamel Erosion and Attrition
Dental erosion, caused by acidic foods or beverages, and attrition, caused by grinding or bruxism, can lead to the progressive loss of enamel. When the enamel layer becomes thin or wears away, the underlying dentin is exposed to external stimuli, leading to hypersensitivity.
- Acidic foods like citrus fruits, carbonated beverages, and wine can dissolve the mineral content of enamel, weakening it and exposing the dentin.
- Tooth wear from bruxism or excessive tooth brushing with abrasive toothpaste can physically degrade enamel and expose dentin.
Abfraction Lesions
Abfraction lesions are mechanical wear defects caused by occlusal forces, often resulting in V-shaped notches at the gum line. These lesions weaken the enamel or cementum near the cervical region of the tooth, exposing the dentinal tubules and resulting in sensitivity.
Tooth Whitening Procedures
Tooth whitening or bleaching procedures often involve the use of peroxide-based agents, which can penetrate the enamel and irritate the dentin-pulp complex. This irritation can lead to temporary or, in some cases, persistent hypersensitivity. The mechanism of bleaching-induced sensitivity is still under research, but it is believed to involve the diffusion of bleaching agents into the dentinal tubules.
Diagnosis of Dentin Hypersensitivity
Proper diagnosis of dentin hypersensitivity is essential, as it can sometimes mimic other dental conditions, such as:
- Cracked tooth syndrome, where a crack in the tooth structure can cause sharp pain.
- Dental caries, which may also cause sensitivity but is generally associated with specific decayed areas.
- Pulpitis, an inflammation of the pulp tissue, often characterized by lingering pain.
Dentists diagnose dentin hypersensitivity through patient history, clinical examination, and sensitivity tests involving controlled stimuli, such as air, cold water, or tactile probing.
Management and Treatment of Dentin Hypersensitivity
The goal of treating dentin hypersensitivity is to reduce or block the response of the dentinal tubules to external stimuli. Treatments fall into two main categories: at-home treatments and professional treatments.
At-Home Treatments
- Desensitizing Toothpastes
- Fluoride Gels or Mouthwashes
- Dietary Modifications
- Proper Oral Hygiene Practices
Desensitizing Toothpastes
These are widely recommended for managing dentin hypersensitivity. They often contain compounds like potassium nitrate, which works by depolarizing the nerve endings in the tubules, reducing pain perception. Other desensitizing agents include strontium chloride and calcium sodium phosphosilicate (NovaMin), which form a layer over the dentin surface, blocking tubule openings.
Fluoride Gels or Mouthwashes
Fluoride has the ability to promote remineralization and can occlude dentinal tubules, reducing sensitivity. Regular use of fluoride-based products can also strengthen the enamel and reduce erosion.
Dietary Modifications
Reducing the intake of acidic foods and beverages can help prevent further erosion of enamel and exposure of dentin.
Proper Oral Hygiene Practices
Using a soft-bristled toothbrush and avoiding aggressive brushing can help protect both the enamel and the gingival tissues, preventing further exposure of dentin.
Professional Treatments
- Fluoride Varnishes
- Dentin Bonding Agents
- Resin-Based Sealants
- Laser Therapy
- Iontophoresis
- Surgical Gum Grafting
Fluoride Varnishes
Dentists may apply concentrated fluoride varnishes to the affected areas, which can reduce sensitivity by enhancing remineralization and forming a protective barrier on the dentin surface.
Dentin Bonding Agents
These materials seal the dentinal tubules and prevent fluid movement, thus reducing sensitivity. Bonding agents are typically used when over-the-counter options are insufficient.
Resin-Based Sealants
Resins can be used to cover exposed dentin, particularly in cases of cervical wear or abfraction lesions. These sealants act as a barrier, preventing stimuli from reaching the dentin-pulp complex.
Laser Therapy
Laser treatments are becoming increasingly popular for treating dentin hypersensitivity. Lasers can alter the nerve fibers within the tubules or melt the tubule ends, sealing them off and reducing fluid movement. Both low-level and high-level lasers have shown promise in reducing sensitivity.
Iontophoresis
This technique involves the use of a mild electrical current to drive fluoride ions deep into the dentinal tubules, promoting tubule occlusion and reducing sensitivity.
Surgical Gum Grafting
In cases of severe gingival recession, gum grafts can cover exposed root dentin, protecting the tooth and reducing sensitivity. This is typically considered a last resort when other treatments have failed.
Advances in Research and Future Directions
Research into dentin hypersensitivity has been advancing, with new materials and techniques being developed to manage this condition more effectively. Recent studies have focused on:
- Biomimetic Materials
- Calcium Phosphate Compounds
- Gene Therapy
- Targeted Nanoparticles
Biomimetic Materials
These materials are designed to mimic the natural mineralization process, promoting the formation of hydroxyapatite or similar minerals within the dentinal tubules. Materials such as bioactive glasses and remineralizing agents are under investigation.
Calcium Phosphate Compounds
Some treatments aim to deliver calcium and phosphate ions directly to the dentin surface, facilitating natural mineralization and tubule occlusion.
Gene Therapy
Although still in experimental stages, gene therapy may one day allow for the regeneration of lost dentin, potentially eliminating hypersensitivity at its root.
Targeted Nanoparticles
These particles can deliver therapeutic agents directly into the dentinal tubules, potentially providing longer-lasting relief than traditional treatments.
Frequently Asked Questions (FAQs)
How can I tell if I have dentin hypersensitivity or another dental issue?
A: Dentin hypersensitivity is characterized by short, sharp pain triggered by specific stimuli (cold, hot, sweet, or touch). If the pain is prolonged, spontaneous, or associated with visible decay or cracks, other dental issues like cavities or pulpitis may be the cause.
Can dentin hypersensitivity go away on its own?
A: In some cases, mild dentin hypersensitivity can diminish over time as the dentinal tubules naturally become blocked by minerals in saliva. However, severe cases usually require treatment.
Are home remedies effective for sensitive teeth?
A: Home remedies like fluoride toothpaste, desensitizing agents, and avoiding acidic foods can help manage mild cases, but professional treatment is often necessary for long-term relief.
Is teeth whitening safe if I have sensitive dentin?
A: Tooth whitening can worsen dentin hypersensitivity. If you have sensitive teeth, consult your dentist before undergoing whitening procedures, and consider desensitizing treatments beforehand.
What is the best toothpaste for sensitive teeth?
A: Toothpaste containing potassium nitrate, stannous fluoride, or NovaMin is effective in reducing dentin hypersensitivity.
Conclusion
Sensitive dentin, or dentin hypersensitivity, is a complex condition rooted in the unique structure and function of dentin within the tooth. Exposure of the dentinal tubules leads to the characteristic pain response seen in hypersensitivity, driven primarily by the hydrodynamic mechanism. Managing this condition requires an understanding of both preventive measures and treatment options, ranging from desensitizing toothpaste and dietary changes to advanced therapies like laser treatments and biomimetic materials. Although challenges remain in effectively managing this condition, ongoing research holds promise for more durable and targeted solutions that can improve the quality of life for those affected by dentin hypersensitivity.