Root canal treatment (RCT) is often conceived as a routine dental procedure; yet, in complex cases, it becomes among the most technically demanding therapies in dentistry. These cases include teeth with unusual, anatomically intricate canal systems, teeth that require retreatment, surgical intervention, regenerative approaches for immature teeth, or management of procedural complications.This article explores each of these areas in detail: complex root canal anatomy, instrumentation, imaging, retreatment, surgical endodontics, biological regenerative techniques, instrumentation adjuncts, complications, and long‑term outcomes.
Table of Contents
ToggleAnatomy & Why ‘Complex’ Matters
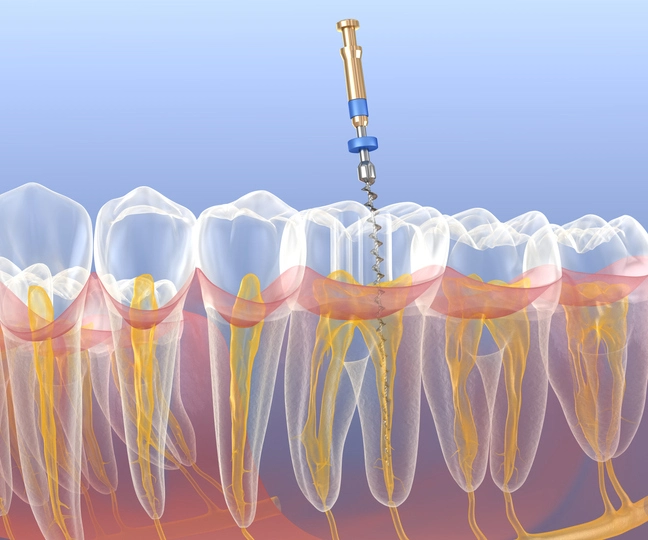
The complexity of RCT often stems from root canal anatomy, especially in the apical third. Canals may be round, oval, elongated, flattened, ribbon‑shaped, or irregularly lobed, often with accessory canals, isthmuses, fins, or lateral branches. These variations make complete mechanical preparation and disinfection extremely challenging.
Understanding anatomical variation is essential: for instance, long oval canals resist full cleaning by circular NiTi files, leaving untreated surfaces in apical regions—a niche for persistent bacteria. Teeth with developmental anomalies (e.g. taurodontism), complex morphology, or calcified canals are inherently difficult.
The Expert Consensus on Difficulty Assessment further underscores that retreatment difficulty often isn’t tied to previous restorations but to anatomic complexity and canal configuration. Complexity also influences risk of procedural errors such as ledging, zipping, perforation, transportation, or file fracture.
Advanced Diagnostic Imaging
Modern complex RCT begins with accurate diagnosis. Conventional periapical radiographs can miss certain canals or anatomical details. Cone‑beam computed tomography (CBCT) provides three‑dimensional imaging that reveals root canal morphology, curvatures, missed canals, apical lesions, resorption, perforations, or proximity to vital structures.
CBCT is increasingly considered the standard of care in complex cases. Magnification tools—dental microscopes and loupes—also significantly increase visualization of fine anatomy, though Cochrane evidence is limited regarding long‑term outcome improvement; professional consensus still favors their use in microsurgical and retreatment procedures.
Biomechanical Preparation & Disinfection
Effective cleaning and shaping in complex anatomy rely on combining mechanical and chemical techniques.
File Systems and Instrumentation
- Hand instrumentation: Techniques such as crown‑down, step‑back, hybrid, balanced‑force filing help negotiate curvature and avoid procedural errors.
- Nickel‑titanium rotary files: Due to superelasticity and shape memory, NiTi files negotiate curved canals with less risk of ledging or follow canal curvature better than stainless steel files. Reciprocating and self‑adjusting file systems help clean irregular geometries (e.g. prolonged oval canals).
Irrigation and Adjunctive Techniques
- No instrument can clean every surface; chemical irrigation is crucial. Sodium hypochlorite (commonly used), often activated via ultrasonic, sonic, or laser agitation, enhances penetration into biofilm‑harbouring anatomies (isthmi, fins, lateral canals).
- Laser‑activated irrigation and ultrasonics are especially valuable in retreatments or narrow anatomical spaces.
Goals (Schilder’s principles)
Maintain cleaning, shaping, and sealing form; remove as much infected tissue as possible; and create a canal shape receptive to dense, permanent obturation.
Retreatment: Challenges & Approach
Why retreat?
Retreatment is necessary when initial therapy fails due to persistent infection, missed anatomy, insufficient cleaning or obturation, or procedural mishaps.
Indications & Planning
Retreatment cases may feature fractured instruments, incomplete obturation, new decay threatening canal space, missed canals, or post‑op apical radiolucencies. Diagnosis relies on periapical eval, CBCT, clinical signs, and history.
Procedure
- Removal of previous filling materials (e.g. gutta‑percha) using solvents, rotary NiTi retreatment files, ultrasonics; complete removal improves success rates.
- Negotiation of complexities: broken file retrieval or bypass techniques, specialized ultrasonics, microscope magnification to locate hidden canals.
Outcomes
Reported success rates of nonsurgical retreatment are approximately 75–88%, generally comparable to primary RCT outcomes when well‑executed. One large systematic review reported ~70.9% success at 2–4 years, increasing to ~83% at 4–6 years, then declining later.
Surgical (Apical) Endodontics in Complex Cases (Periradicular Surgery)
When nonsurgical retreatment isn’t feasible or fails, periradicular surgery (apicoectomy) is indicated.
Planning & Assessment
A thorough pre‑surgical CBCT and clinical exam assess bone thickness, anatomical risks (e.g. sinus, nerve), canal morphology, and presence of residual pathology.
Procedure
- Local anesthesia (e.g. 2% lidocaine with adrenaline for haemostasis)
- Design and elevation of a surgical flap (envelope, triangular, semilunar, etc.)
- Resection of apical 3 mm of root, removal of pathosis, root‑end cavity prep and retrofill using MTA or bioceramics
- Achieve haemostasis, irrigation, closure, and suturing
- Post‑operative care includes ice, analgesia, antimicrobial rinse, suture removal in 2–4 days.
Outcomes & Complications
Success is defined clinically (symptom resolution) and radiographically (bone re‑formation). If unsuccessful, retreat surgery has lower success (~35%), and options include monitoring, extraction, or further retreatment. Common complications include bleeding, swelling, infection, nerve damage, or sinus involvement.
Regenerative & Apexification Techniques for Immature or Open‑Apex Teeth
Immature permanent teeth with open apices and necrotic pulp present unique challenges. Traditional root canal filling is impossible without an apical stop.
Apexification
A process to induce calcific barrier at apex using calcium hydroxide or MTA/Biodentine. This often requires multiple appointments over months. Reported success ranges from ~74–100% depending on material used.
Regenerative Endodontics
Also known as pulp revascularization, this strategy aims to stimulate continued root development by disinfecting canal space, placing scaffolding/bio‑stimulating materials, and sealing to allow ingrowth of vital tissue. While data are still evolving, they offer tooth preservation in young patients.
Instrument Separation & Procedural Errors: Prevention & Management
Instrument fracture (file separation) is a frequent complication, especially in narrow, curved, calcified canals. Factors include canal curvature, repeated use of NiTi files, cyclic fatigue, inadequate glide path, and over‑torque.
Prevention strategies:
- Create straight‑line access
- Glide path with small hand files
- Follow manufacturers’ torque and speed guidelines
- Single‑use protocols
- Regular inspection of files for metal fatigue.
Management:
- Attempt to retrieve or bypass broken fragments under magnification and ultrasonics
- If removal risks damage, carefully obturate to circumvent fragment
- Consider surgical endodontics if inaccessible, or extraction if prognosis poor
Technologies & Emerging Innovations
New technologies are increasingly applied to manage complexity:
- Robot‑assisted endodontics: e.g. DentiBot, a system capable of 6‑DoF force control to adjust file path in real time and protect against fracture.
- Future directions include AI‑assisted planning, guided endodontics, and improved bio‑materials for regenerative approaches.
Post‑operative Care & Long‑Term Prognosis
After treatment, placing a definitive coronal restoration—often a crown—is crucial to prevent reinfection. The restoration restores function, seals the tooth, and supports structural integrity.
Follow‑up radiographs at 6–12 months then annually allow clinicians to monitor periapical healing. Success is gauged clinically (no pain, swelling, sinus tract) and radiographically (resolution of radiolucency).
Prognosis depends on case type and treatment quality. Primary RCT success rates exceed 85–90% in standard cases; retreatment and surgical interventions vary but remain high if performed in specialist hands.
Summary & Take‑Home Messages
- Complex root canals pose challenges due to variations in anatomy, procedural complications, previous treatment failures, surgery, or immature teeth.
- Successful management relies on advanced diagnostics (CBCT, magnification), sophisticated instrumentation (NiTi rotary/reciprocating, ultrasonics, lasers), and chemical disinfection.
- Retreatment when initial treatment fails requires complete removal of prior materials, careful negotiation of anatomy, and predictable techniques that yield ~75–88% success.
- Periradicular (surgical) intervention is reserved for non‑restorable cases by retreatment, with success contingent on surgical planning and technique.
- Regenerative or apexification techniques allow treatment in immature teeth using bioceramics and scaffolding materials.
- Prevention and management of procedural errors (e.g. instrument separation) are critical—supported by contemporary protocols and preventive workflows.
- Emerging technologies like robotics and guided planning promise even greater precision in the future.
- Ultimately, complex RCTs demand specialist skill, meticulous technique, thorough planning, and appropriate follow-up care to save teeth and optimize patient outcomes.
Final Thoughts
Complex root canal treatments embody the intersection of anatomy, technology, microbiology, and clinical skill. When conventional approaches fall short, endodontic retreatment, surgical techniques, regenerative protocols, and emerging technology provide sophisticated tools to preserve natural teeth that might otherwise be lost.