Attention-Deficit/Hyperactivity Disorder (ADHD) is a complex neurodevelopmental condition characterized by persistent patterns of inattention, hyperactivity, and impulsivity. It affects children and adults alike, often impacting school performance, career progression, relationships, and self-esteem. While ADHD is commonly diagnosed during childhood, a significant number of individuals continue to experience symptoms into adulthood. This article provides an in-depth look into ADHD, exploring its history, causes, symptoms, diagnosis, treatment options, and coping mechanisms.
Table of Contents
ToggleHistory and Evolution of ADHD
ADHD has been known by various names throughout history. In the early 1900s, it was referred to as “minimal brain dysfunction.” Over time, as understanding evolved, the condition went through several redefinitions:
- 1980 (DSM-III): Introduced Attention Deficit Disorder (ADD) with or without hyperactivity.
- 1987 (DSM-III-R): The term ADHD replaced ADD, combining inattentive and hyperactive symptoms.
- Present Day: The DSM-5 categorizes ADHD into three distinct presentations: inattentive, hyperactive-impulsive, and combined.
Prevalence and Demographic Distribution
ADHD is among the most commonly diagnosed childhood mental health disorders. Globally, around 5-7% of children are estimated to have ADHD. In the U.S., approximately 9.4% of children aged 2–17 have been diagnosed.
- Gender Differences: Boys are more frequently diagnosed than girls. However, girls are more likely to present with inattentive symptoms, which are often underrecognized.
- Adult ADHD: An estimated 2.5-4.4% of adults live with ADHD, many undiagnosed or misdiagnosed earlier in life.
Causes of ADHD
The origins of ADHD are multifactorial, involving both genetic and environmental influences:
- Genetics: ADHD tends to run in families. Studies estimate a heritability rate of about 74%.
- Prenatal and Perinatal Factors: Exposure to tobacco, alcohol, or drugs during pregnancy, premature birth, and low birth weight increase the risk.
- Environmental Influences: Lead exposure, poor nutrition, and early trauma may contribute.
- Neurological Differences: Brain imaging shows that individuals with ADHD often have differences in the prefrontal cortex and in neurotransmitter activity, particularly involving dopamine and norepinephrine.
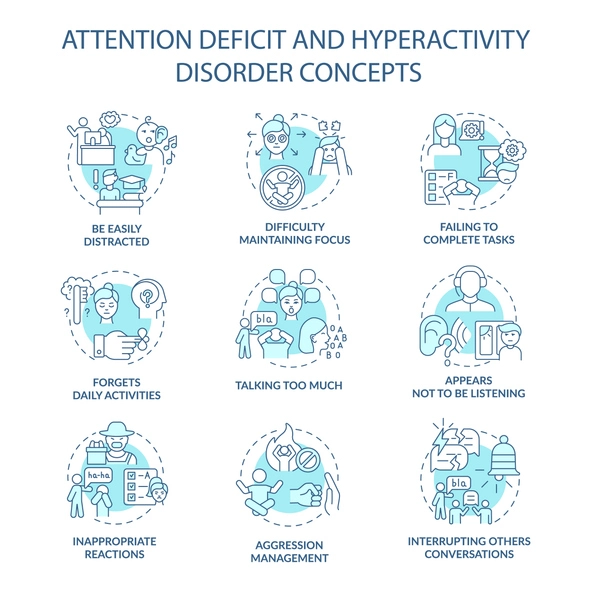
Types of ADHD and Core Symptoms
The DSM-5 outlines three presentations of ADHD, each with distinct characteristics:
A. Predominantly Inattentive Presentation
- Fails to give close attention to details
- Difficulty sustaining attention in tasks or play
- Frequently loses items necessary for tasks
- Avoids tasks requiring sustained mental effort
B. Predominantly Hyperactive-Impulsive Presentation
- Fidgets or squirms in seat
- Leaves seat in inappropriate situations
- Talks excessively
- Interrupts or intrudes on others
C. Combined Presentation
Features both inattentive and hyperactive impulsive symptoms.
Symptoms must:
- Last for at least six months
- Be inappropriate for developmental level
- Appear before age 12
- Cause impairment in social, academic, or occupational settings
Diagnosis and Evaluation
Diagnosing ADHD involves a multi-step process:
Clinical Evaluation
- Comprehensive interviews with the patient, parents, and teachers
- Use of standardized rating scales (e.g., Conners, Vanderbilt, or SNAP-IV)
Differential Diagnosis
ADHD shares symptoms with other conditions, which must be ruled out:
- Anxiety disorders
- Depression
- Learning disabilities
- Autism spectrum disorder
Observation
Input from teachers and caregivers helps assess symptoms in various environments.
ADHD Across Different Life Stages
Childhood
Symptoms are typically more visible and disruptive (e.g., running, climbing, disobedience).
Adolescence
Hyperactivity often diminishes, but inattention and impulsivity may intensify due to increasing academic and social demands.
Adulthood
Difficulties may shift toward poor time management, disorganization, and unstable relationships. Adults with ADHD may experience lower job satisfaction and higher job turnover.
Common Comorbidities
ADHD often coexists with other mental health and developmental disorders:
- Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD)
- Anxiety Disorders
- Major Depressive Disorder
- Bipolar Disorder
- Learning Disabilities (e.g., dyslexia, dyscalculia)
- Autism Spectrum Disorder (ASD)
Treating comorbid conditions is crucial for improving overall functioning and treatment success.
Treatment Options for ADHD
Management of ADHD typically involves a combination of approaches tailored to individual needs:
A. Medication
- Stimulants: Methylphenidate (Ritalin, Concerta) and amphetamines (Adderall, Vyvanse) are first-line treatments.
- Non-stimulants: Atomoxetine (Strattera), guanfacine (Intuniv), and clonidine can be alternatives or add-ons.
B. Behavioral Interventions
- Parent training in behavior management
- Classroom behavior management plans
- Token economies and reward systems
C. Educational Support
- 504 Plans and IEPs: Provide academic accommodations such as extended test times or modified assignments.
- School counseling and special education support
D. Psychotherapy
Cognitive Behavioral Therapy (CBT): Helps improve organizational skills, emotional regulation, and coping strategies.
E. Lifestyle and Home Strategies
- Consistent daily routines
- Visual schedules and task organizers
- Balanced nutrition and physical activity
- Reducing screen time and improving sleep hygiene
Living with ADHD: Practical Coping Strategies
For Children
- Positive reinforcement and clear expectations
- Visual aids and structured environments
- Social skills training
For Adolescents
- Encouraging self-advocacy and independence
- Monitoring time usage and academic tasks
For Adults
- Using planners, reminders, and organizational apps
- Seeking workplace accommodations
- Participating in ADHD coaching or support groups
Advocacy and Social Impact
Public awareness about ADHD has improved, but stigma and misunderstanding persist. Advocacy groups work toward:
- Promoting early and accurate diagnosis
- Encouraging inclusive education and workplace practices
- Shifting societal perception from deficit to neurodiversity
Celebrating strengths like creativity, hyperfocus, and resilience can empower individuals with ADHD.
Future Directions and Emerging Research
Areas of Ongoing Research:
- Neuroimaging and Biomarkers: For objective diagnosis tools
- Digital Therapeutics: Apps and games targeting executive function
- Nutritional Studies: Exploring the role of omega-3, iron, and zinc
- Gender and Cultural Differences: Improving diagnosis across diverse populations
As our understanding deepens, more personalized, effective treatments are anticipated.
Conclusion
ADHD is a lifelong condition that can be managed with proper understanding, support, and intervention. Early diagnosis, individualized treatment, and societal support can help those with ADHD lead fulfilling lives. Continued advocacy and research are crucial for fostering a compassionate and informed society that embraces neurodiversity and empowers all individuals to thrive.