Acid reflux, also known as gastroesophageal reflux disease (GERD), is a common condition characterized by the backward flow of stomach acid into the esophagus. This condition often manifests as heartburn, regurgitation, and other gastrointestinal symptoms. However, less commonly discussed is how acid reflux can significantly impact oral health, particularly the teeth. Over time, the acidic nature of the reflux can erode tooth enamel, leading to a range of dental problems. This article explores the connection between acid reflux and dental health, the mechanisms involved, and strategies for prevention and management.
Table of Contents
ToggleWhat is Acid Reflux?
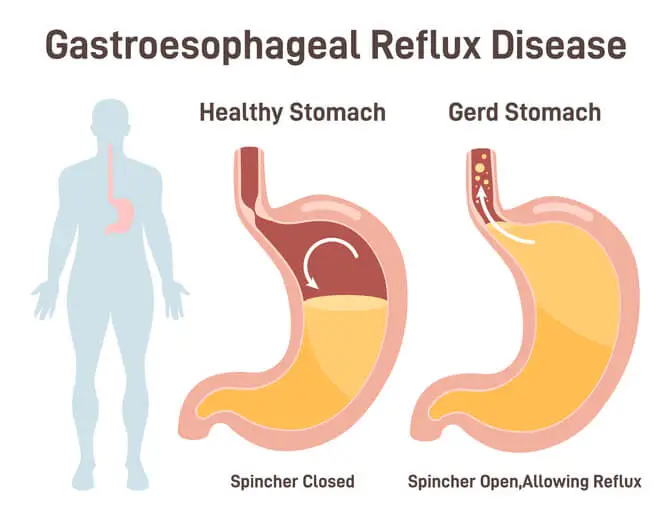
Acid reflux occurs when the lower esophageal sphincter (LES), a ring of muscle that acts as a valve between the stomach and esophagus, becomes weakened or relaxes inappropriately. This allows stomach contents, including hydrochloric acid, to flow back into the esophagus. While occasional reflux is normal, chronic reflux—referred to as GERD—requires medical attention.
Symptoms of Acid Reflux
- Heartburn: A burning sensation in the chest, often after eating or at night.
- Regurgitation: The sensation of acid or food backing up into the throat or mouth.
- Dysphagia: Difficulty swallowing due to irritation or narrowing of the esophagus.
- Chronic cough: Caused by irritation in the respiratory tract from refluxed acid.
- Dental issues: Increased sensitivity, discoloration, and enamel erosion.
The Role of Stomach Acid in Dental Erosion
The primary way acid reflux affects the teeth is through acid erosion. Hydrochloric acid in the stomach is vital for digestion but is highly corrosive. When it reaches the oral cavity during reflux episodes, it can erode the outer layer of the teeth, known as enamel. Enamel is the hardest substance in the human body, but it is not immune to prolonged exposure to acid.
How Acid Reflux Affects Teeth
- Enamel Erosion: Repeated exposure to stomach acid weakens enamel, making it thinner and more prone to damage. Enamel erosion is irreversible, leaving the underlying dentin exposed.
- Increased Sensitivity: As enamel erodes, the dentin beneath becomes exposed, leading to dentin hypersensitivity to hot, cold, and sweet stimuli.
- Discoloration: Enamel erosion may cause teeth to appear yellow or darker because dentin has a natural yellow hue.
- Increased Risk of Cavities: Weakened enamel is less effective at protecting teeth from bacteria, increasing the likelihood of cavities and tooth decay.
- Structural Damage: In severe cases, prolonged acid exposure can lead to cracks, chips, and even tooth loss.
Signs of Acid-Related Dental Erosion
Dental erosion caused by acid reflux often goes unnoticed in its early stages. However, there are telltale signs that patients and dentists can look for:
- Smooth, shiny surfaces on teeth that indicate enamel loss.
- Flat or worn teeth, especially on the chewing surfaces.
- Cupping or craters on the surface of molars.
- Increased transparency, particularly on the edges of the front teeth.
- Tooth sensitivity that worsens over time.
Dentists are often the first healthcare professionals to identify acid reflux-related dental issues, as these symptoms can develop before other signs of GERD become apparent.
Risk Factors for Acid Reflux and Dental Erosion
Certain lifestyle factors and medical conditions increase the risk of acid reflux and its impact on dental health:
- Dietary Habits: Consuming acidic foods and beverages (e.g., citrus fruits, sodas, and coffee) exacerbates the effects of reflux on enamel.
- Obesity: Excess abdominal pressure can push stomach contents upward into the esophagus.
- Smoking: Smoking weakens the LES and increases acid production in the stomach.
- Medications: Certain medications, such as anticholinergics, calcium channel blockers, and sedatives, can relax the LES.
- Pregnancy: Hormonal changes and increased abdominal pressure can lead to reflux.
- Chronic conditions: Conditions such as hiatal hernia, diabetes, and delayed stomach emptying (gastroparesis) are associated with GERD.
The Role of Saliva in Neutralizing Acid
Saliva plays a crucial role in protecting teeth from acid erosion. It helps neutralize acid, washes away food particles, and provides minerals that aid in the remineralization of enamel. However, acid reflux can reduce saliva production or overwhelm its protective capabilities, increasing the risk of dental damage.
Complications of Acid Reflux on Oral Health
The dental impacts of acid reflux extend beyond enamel erosion:
- Periodontal Disease: Acid reflux can cause inflammation in the oral cavity, contributing to gum disease.
- Oral Mucosal Irritation: Stomach acid can irritate the soft tissues of the mouth, leading to sores or ulcers.
- Halitosis (Bad Breath): Chronic acid reflux may result in foul-smelling breath due to regurgitated stomach contents.
- Bruxism: Some individuals develop bruxism (teeth grinding) as a response to discomfort caused by GERD, which can further damage enamel.
Prevention and Management of Acid Reflux-Induced Dental Damage
Managing the oral health impacts of acid reflux involves addressing both the underlying reflux condition and its effects on teeth. Here are steps to prevent and minimize damage:
Medical Management of GERD
- Medications: Proton pump inhibitors (PPIs), H2 receptor blockers, and antacids can reduce stomach acid production and alleviate reflux symptoms.
- Lifestyle Modifications:
- Eat smaller meals and avoid eating late at night.
- Elevate the head of the bed to reduce nighttime reflux.
- Avoid trigger foods such as spicy, fatty, or acidic items.
- Weight Management: Losing weight can reduce abdominal pressure and GERD symptoms.
Dental Care Strategies
- Fluoride Treatments: Dentists may apply fluoride varnishes or prescribe fluoride toothpaste to strengthen enamel.
- Remineralizing Products: Products containing calcium and phosphate can help repair early enamel damage.
- Mouthguards: Custom nightguards can protect teeth from bruxism associated with GERD.
- Regular Dental Visits: Routine check-ups allow for early detection and management of dental erosion.
Dietary Considerations
- Limit acidic foods and beverages.
- Drink water after meals to rinse away acid.
- Chew sugar-free gum to stimulate saliva production.
Oral Hygiene Practices
- Avoid brushing immediately after a reflux episode, as enamel is softened and more susceptible to damage. Instead, rinse with water or a fluoride mouthwash.
- Use a soft bristled toothbrush and non-abrasive toothpaste to minimize wear on enamel.
When to Seek Professional Help
If you experience frequent heartburn, regurgitation, or dental symptoms such as sensitivity and discoloration, consult both a gastroenterologist and a dentist. Addressing acid reflux early can prevent severe complications for both your digestive and oral health.
Frequently Asked Questions (FAQs)
1. Can acid reflux permanently damage my teeth?
Yes, acid reflux can cause permanent enamel erosion. Once enamel is lost, it does not regenerate, which is why prevention and early intervention are essential.
2. How can I tell if acid reflux is affecting my teeth?
Common signs include increased tooth sensitivity, yellowing teeth, smooth or worn-down enamel, and small pits or craters on the molars.
3. Can drinking water help with acid reflux?
Yes, drinking water helps wash away acid and neutralize its effects. Alkaline water, in particular, may help reduce acidity in the mouth.
4. Should I brush my teeth immediately after acid reflux?
No. Brushing immediately after an acid reflux episode can worsen enamel erosion. Instead, rinse your mouth with water or a fluoride mouthwash and wait at least 30 minutes before brushing.
5. Can chewing gum help with acid reflux?
Yes, sugar-free gum stimulates saliva production, which helps neutralize acid and protect enamel.
Conclusion
Acid reflux is more than just an uncomfortable digestive issue; it has far-reaching effects on oral health, particularly the teeth. Enamel erosion caused by acid exposure can lead to sensitivity, discoloration, and a heightened risk of cavities. Understanding the connection between GERD and dental health underscores the importance of early intervention, proper management, and preventive care.
By working collaboratively with healthcare providers and maintaining good oral hygiene, individuals with acid reflux can protect their teeth and overall oral health from the damaging effects of stomach acid. Taking a proactive approach ensures that both your smile and digestive system remain in optimal condition.