Trigeminal neuralgia (TN), often described as one of the most painful conditions known to humanity, is a chronic disorder that affects the trigeminal nerve—the fifth cranial nerve responsible for transmitting facial sensations to the brain. This condition is characterized by sudden, intense facial pain, which can be triggered by everyday activities such as speaking, chewing, or even the sensation of a breeze on the face.
The condition has been recognized for centuries, but its underlying mechanisms and treatment options have only recently been understood more comprehensively. This article delves into the nature of trigeminal neuralgia, its causes, symptoms, diagnostic processes, and treatment approaches.
Table of Contents
ToggleAnatomy of the Trigeminal Nerve
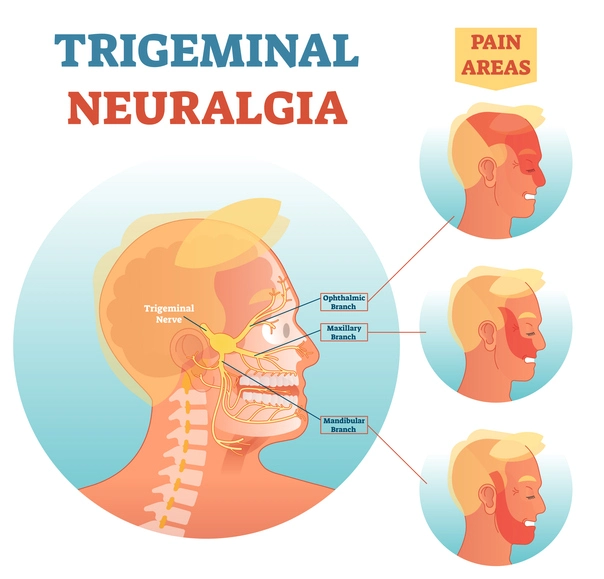
The trigeminal nerve is one of the largest cranial nerves, with three primary branches:
- Ophthalmic branch (V1) – Supplies sensation to the upper part of the face, including the forehead, scalp, and eyes.
- Maxillary branch (V2) – Covers the middle section of the face, including the cheeks, upper lip, and upper teeth.
- Mandibular branch (V3) – Innervates the lower face, including the jaw, lower lip, and lower teeth, and controls some motor functions for chewing.
In trigeminal neuralgia, one or more of these branches are affected, leading to the characteristic episodes of facial pain.
Symptoms of Trigeminal Neuralgia
The hallmark of TN is intense, sudden facial pain that can last from a few seconds to a couple of minutes. This pain is often described as electric shock like or stabbing and occurs in paroxysms. Key characteristics include:
- Location – Pain usually affects one side of the face, corresponding to one or more branches of the trigeminal nerve.
- Triggers – Everyday activities such as talking, eating, brushing teeth, or even exposure to wind can provoke an attack.
- Duration and Intensity – Pain episodes are brief but excruciating, often recurring in quick succession.
- Refractory Period – Between attacks, patients may experience a refractory period during which pain does not occur.
- Progression – Over time, pain episodes may become more frequent and less responsive to triggers.
Some patients may develop a continuous, aching pain between episodes, referred to as atypical trigeminal neuralgia.
Causes of Trigeminal Neuralgia
The exact cause of TN varies, but it is generally classified into two types: primary (idiopathic) and secondary.
Primary (Classic) Trigeminal Neuralgia
In classic TN, no underlying structural cause is found, but it is often linked to compression of the trigeminal nerve root by a blood vessel. This compression leads to irritation and demyelination of the nerve, resulting in abnormal transmission of pain signals.
Secondary Trigeminal Neuralgia
Secondary TN arises from identifiable structural lesions or diseases affecting the trigeminal nerve, such as:
- Multiple sclerosis (MS) – Demyelination caused by MS can affect the trigeminal nerve, leading to pain.
- Tumors – Space occupying lesions near the brainstem or along the nerve’s path can compress or damage the nerve.
- Trauma – Facial or cranial injuries may contribute to nerve damage.
- Infections – Conditions like shingles (herpes zoster) can involve the trigeminal nerve, resulting in pain.
Risk Factors
While TN can occur in anyone, certain factors increase susceptibility:
- Age – TN is more common in people over 50 years old, although younger individuals can also be affected.
- Gender – Women are more likely to develop TN than men.
- Family History – A genetic predisposition may exist, particularly in cases of familial TN.
- Neurological Conditions – Diseases like multiple sclerosis significantly raise the risk.
Diagnosis
Diagnosing trigeminal neuralgia involves a thorough medical history and physical examination. Since no specific test confirms TN, diagnosis is largely clinical, based on symptoms and exclusion of other causes.
- Medical History
- Imaging Studies
- Neurological Examination
Medical History
Doctors will assess:
- Nature, location, and intensity of the pain.
- Triggers and duration of episodes.
- Any accompanying neurological symptoms.
Imaging Studies
Imaging techniques like magnetic resonance imaging (MRI) are crucial to rule out secondary causes such as tumors or multiple sclerosis.
Neurological Examination
A detailed examination helps identify sensory or motor deficits that might suggest an underlying condition.
Differential Diagnosis
Several conditions can mimic trigeminal neuralgia, making accurate diagnosis essential:
- Dental Issues – Tooth infections or abscesses.
- Migraine or Cluster Headaches – Severe head pain that can involve the face.
- Postherpetic Neuralgia – Persistent pain following a shingles outbreak.
- Temporomandibular Joint (TMJ) Disorders – Jaw joint dysfunction causing facial pain.
Treatment Options for Trigeminal Neuralgia
Managing trigeminal neuralgia focuses on relieving pain and improving quality of life. Treatment options range from medications to surgical interventions.
- Medications
- Nerve Blocks and Injections
- Surgical Interventions
Medications
Pharmacological treatment is often the first line of therapy.
- Anticonvulsants – Medications like carbamazepine and oxcarbazepine are commonly used and highly effective. They work by stabilizing nerve activity.
- Muscle Relaxants – Baclofen can be used alone or in combination with anticonvulsants.
- Tricyclic Antidepressants – Low doses of drugs like amitriptyline are beneficial for atypical facial pain.
- Pain Relievers – Standard analgesics are typically ineffective for TN.
Nerve Blocks and Injections
- Local Anesthetic Injections – Temporarily block pain by numbing the affected nerve.
- Botulinum Toxin (Botox) – Emerging evidence suggests Botox injections may reduce pain by inhibiting nerve activity.
Surgical Interventions
Surgery is considered for patients who do not respond to medications or experience intolerable side effects.
- Microvascular Decompression (MVD) – A highly effective procedure that involves repositioning or removing blood vessels compressing the trigeminal nerve.
- Radiofrequency Rhizotomy – A minimally invasive procedure that selectively destroys nerve fibers to reduce pain.
- Gamma Knife Radiosurgery – A non-invasive option that uses focused radiation to damage the trigeminal nerve.
- Balloon Compression – A catheter inflates a balloon near the nerve to disrupt pain signals.
Emerging Therapies
Recent advancements are exploring novel approaches for TN management:
- Neuromodulation – Techniques like transcranial magnetic stimulation (TMS) show promise in modulating nerve activity.
- Gene Therapy – Experimental research is targeting genetic pathways involved in pain transmission.
Living with Trigeminal Neuralgia
Coping with TN involves a holistic approach that addresses physical, emotional, and social aspects. Support groups, counseling, and stress management techniques can help patients navigate the challenges of living with chronic pain.
Diet and Lifestyle Changes
Avoiding known triggers and maintaining a healthy lifestyle can reduce the frequency of attacks. Gentle exercises, relaxation techniques, and a balanced diet may also provide benefits.
Support Systems
Connecting with others who understand the condition can provide emotional relief. Organizations such as the Trigeminal Neuralgia Association offer resources and support.
Prognosis for Trigeminal Neuralgia
The prognosis for TN varies. While some patients experience significant relief with treatment, others may struggle with recurrent or refractory pain. Advances in surgical techniques and medications continue to improve outcomes, offering hope for better management.
Frequently Asked Questions (FAQs)
Is trigeminal neuralgia life-threatening?
No, TN itself is not life-threatening, but the intense pain can severely affect a person’s quality of life. In rare cases, the distress from chronic pain can lead to depression or anxiety.
What triggers trigeminal neuralgia pain?
Common triggers include:
- Eating, chewing, or drinking
- Brushing teeth
- Talking or smiling
- Touching the face
- Cold air or wind exposure
Can trigeminal neuralgia go away on its own?
TN symptoms may go into remission (pain-free periods), but the condition often returns. Without treatment, episodes may become more frequent and severe over time.
How long do TN attacks last?
Each episode can last from a few seconds to two minutes. Multiple attacks can occur in clusters throughout the day.
What is the best treatment for trigeminal neuralgia?
The best treatment varies for each person. Medications like carbamazepine are the first-line treatment. If medications fail, surgical procedures like microvascular decompression or Gamma Knife radiosurgery may be considered.
Can diet or lifestyle changes help?
While diet alone cannot cure TN, avoiding triggers (caffeine, spicy foods, and cold drinks) may help reduce attacks. Managing stress and using relaxation techniques can also help.
Is trigeminal neuralgia a symptom of multiple sclerosis?
In some cases, TN is an early symptom of MS, as the disease can damage the protective covering (myelin) of the trigeminal nerve. However, most people with TN do not have MS.
Is there a cure for trigeminal neuralgia?
There is no permanent cure, but many treatments can significantly reduce or eliminate pain. Some people experience long-term relief after microvascular decompression surgery or Gamma Knife treatment.
Can trigeminal neuralgia affect both sides of the face?
Yes, but it is rare. When TN affects both sides, it is referred to as bilateral trigeminal neuralgia, which is sometimes linked to multiple sclerosis.
Does trigeminal neuralgia worsen over time?
For many patients, TN becomes more frequent and severe over time. This is why early diagnosis and treatment are essential to manage symptoms effectively.
Conclusion
Trigeminal neuralgia is a debilitating condition that significantly impacts the lives of those it affects. Understanding the condition’s causes, symptoms, and treatment options is crucial for patients and healthcare providers alike. While the journey to finding effective management can be challenging, ongoing research and emerging therapies provide a bright horizon for individuals living with this “suicide disease.”
By raising awareness and fostering empathy, society can better support those facing the daily struggles of trigeminal neuralgia. With timely diagnosis, personalized treatment, and comprehensive care, it is possible to reclaim a better quality of life.