Sterilization is a critical aspect of dental practice, ensuring the safety and well-being of both patients and dental professionals. In the dental environment, where instruments and equipment come into direct contact with bodily fluids, rigorous sterilization protocols are essential to prevent cross-contamination and the spread of infectious diseases. This article explores the various sterilization techniques employed in dentistry, emphasizing their importance, methods, and implementation in clinical practice.
Table of Contents
ToggleImportance of Sterilization in Dentistry
Dental field is particularly susceptible to the transmission of infectious agents due to the invasive nature of many procedures. Instruments often come into contact with saliva, blood, and other potentially infectious materials. Without proper sterilization, these instruments can become vectors for pathogens such as bacteria, viruses, and fungi, leading to infections and diseases, including hepatitis B and C, HIV, and tuberculosis.
Ensuring proper sterilization in dentistry is not only a regulatory requirement but also a moral and ethical obligation to protect patient health. It enhances patient confidence in dental services and maintains the professional integrity of the dental practice.
Principles of Sterilization
Sterilization involves the complete elimination or destruction of all forms of microbial life, including bacterial spores, which are the most resistant form of microorganisms. The key principles of sterilization in dentistry include:
- Cleaning: The removal of visible debris and organic matter from instruments.
- Disinfection: The elimination of most pathogenic microorganisms, except bacterial spores, on inanimate objects.
- Sterilization: The destruction of all forms of microbial life.
Common Sterilization Techniques in Dentistry
Several sterilization methods are utilized in dentistry, each with specific applications, advantages, and limitations. The choice of sterilization method depends on the type of instruments, materials, and the extent of contamination.
- Autoclaving (Steam Sterilization)
- Dry Heat Sterilization
- Chemical Vapor Sterilization
- Ethylene Oxide Sterilization
- Cold Sterilization
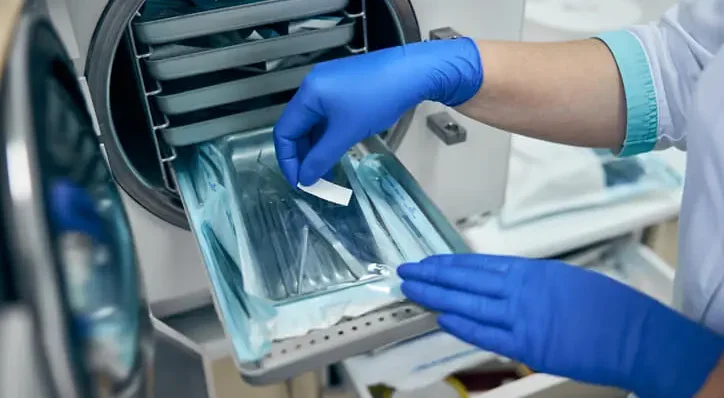
Autoclaving (Steam Sterilization)
Autoclaving is the most widely used method for sterilizing dental instruments. It involves using steam under pressure to achieve high temperatures that destroy all microorganisms, including spores. The typical parameters for autoclaving are 121°C (250°F) at 15 psi for 15-20 minutes or 134°C (273°F) at 30 psi for 3-5 minutes.
Advantages
- Highly effective at killing all microorganisms.
- Time-efficient.
- Suitable for most dental instruments.
Limitations
- Not suitable for heat-sensitive instruments.
- Requires proper maintenance and validation to ensure effectiveness.
Procedure
- Instruments are cleaned to remove any organic debris.
- Packaged in sterilization pouches or wrapped in sterile cloth.
- Placed in the autoclave chamber and subjected to the sterilization cycle.
- After the cycle, instruments are dried and stored in a sterile environment.
Dry Heat Sterilization
Dry heat sterilization involves using hot air that is either static or circulated to kill microorganisms. The typical temperature settings are 160°C (320°F) for 2 hours or 170°C (340°F) for 1 hour.
Advantages
- Suitable for instruments that might be damaged by moist heat.
- No risk of corrosion for metal instruments.
Limitations
- Longer sterilization times compared to autoclaving.
- Not suitable for heat-sensitive items or materials that can be damaged by high temperatures.
Procedure
- Instruments are cleaned and dried.
- Placed in a dry heat sterilizer and subjected to the required temperature and time.
- After sterilization, instruments are cooled and stored properly.
Chemical Vapor Sterilization
This method uses a combination of chemicals such as alcohol, formaldehyde, and acetone, heated under pressure to produce a sterilizing gas. The typical parameters are 132°C (270°F) at 20 psi for 20 minutes.
Advantages
- Shorter cycle time compared to dry heat sterilization.
- Suitable for instruments that cannot withstand steam sterilization.
Limitations
- Requires proper ventilation due to the release of toxic vapors.
- Chemicals can be hazardous to health if not handled properly.
Procedure
- Instruments are cleaned and dried.
- Placed in a chemical vapor sterilizer and exposed to the chemical mixture at the required parameters.
- After sterilization, instruments are aired out to remove any residual chemical fumes before use.
Ethylene Oxide Sterilization
Ethylene oxide gas is used for sterilizing heat-sensitive and moisture-sensitive instruments. This method operates at lower temperatures, around 37-63°C (99-145°F).
Advantages
- Effective for complex and delicate instruments.
- Low-temperature process suitable for a wide range of materials.
Limitations
- Lengthy sterilization and aeration times.
- Requires strict handling protocols due to the toxic and explosive nature of ethylene oxide.
Procedure
- Instruments are cleaned and dried.
- Placed in a sterilization chamber and exposed to ethylene oxide gas for several hours.
- Followed by an aeration period to remove any residual gas.
Cold Sterilization
Cold sterilization involves the use of liquid chemical agents, such as glutaraldehyde or hydrogen peroxide, to sterilize instruments at room temperature.
Advantages
- Suitable for heat-sensitive instruments.
- Can be used for instruments that cannot be autoclaved or exposed to high temperatures.
Limitations
- Longer contact time required for complete sterilization.
- Potential for chemical residue on instruments.
Procedure
- Instruments are thoroughly cleaned and dried.
- Submerged in a sterilant solution for the required contact time (typically 10-12 hours).
- Rinsed with sterile water and dried before use.
Implementation of Sterilization Protocols in Dental Practices
Effective implementation of sterilization protocols requires adherence to a structured approach involving several key steps:
- Instrument Processing Area Design
- Instrument Cleaning
- Packaging
- Sterilization
- Storage
- Record Keeping
Instrument Processing Area Design
- Designated areas for cleaning, disinfecting, packaging, and sterilizing instruments.
- Separate “dirty” and “clean” zones to prevent cross-contamination.
Instrument Cleaning
- Pre-cleaning by rinsing instruments immediately after use.
- Use of ultrasonic cleaners or automated washer-disinfectors to remove debris.
- Manual cleaning with brushes for difficult-to-reach areas.
Packaging
- Use of appropriate packaging materials such as sterilization pouches or wraps.
- Proper labeling with the date of sterilization and batch number.
Sterilization
- Selection of the appropriate sterilization method based on the type of instrument.
- Adherence to manufacturer guidelines for sterilizer operation.
- Regular monitoring and validation of sterilizer performance using biological, chemical, and mechanical indicators.
Storage
- Sterilized instruments should be stored in a clean, dry, and protected environment.
- Avoiding exposure to moisture or contamination.
Record Keeping
- Maintaining detailed records of sterilization cycles, including date, method, and results of monitoring tests.
- Regular audits to ensure compliance with sterilization protocols.
Challenges and Considerations
Despite the advances in sterilization technology, dental practices face several challenges in ensuring effective sterilization:
- Compliance and Training
- Maintenance and Validation
- Cost
- Handling and Storage
Compliance and Training
Ensuring all staff members are adequately trained and consistently follow sterilization protocols.
Maintenance and Validation
Regular maintenance and validation of sterilization equipment to ensure its proper functioning.
Cost
Investing in advanced sterilization equipment and maintaining it can be costly.
Handling and Storage
Proper handling and storage of sterilized instruments to prevent recontamination.
Frequently Asked Questions (FAQs)
What are the 7 methods of sterilization?
Sterilization is the process of eliminating all forms of microbial life, including bacteria, viruses, fungi, and spores. The seven methods of sterilization commonly used in healthcare and dental settings are:
Autoclaving (Steam Sterilization):
- Uses pressurized steam at high temperatures (121–134°C) to kill microorganisms.
- Most commonly used in dental and medical practices due to its efficiency.
Dry Heat Sterilization:
- Uses high temperatures (160–190°C) for prolonged periods (1–2 hours).
- Ideal for instruments that cannot withstand moisture, such as metal tools.
Chemical Sterilization:
- Uses chemical agents like ethylene oxide (EtO), hydrogen peroxide, or formaldehyde gas.
- Suitable for heat-sensitive instruments and materials.
Radiation Sterilization:
- Uses gamma rays or electron beams to destroy microorganisms.
- Commonly used for medical supplies, pharmaceuticals, and disposable dental products.
Filtration Sterilization:
- Used for sterilizing liquids and air by passing them through specialized filters that trap microorganisms.
- Common in laboratory settings and pharmaceutical manufacturing.
Gas Plasma Sterilization:
- Uses hydrogen peroxide plasma to sterilize instruments quickly at low temperatures.
- An alternative to EtO sterilization with fewer toxic byproducts.
Cold Sterilization:
- Involves soaking instruments in chemical solutions such as glutaraldehyde for extended periods.
- Used for heat-sensitive items but requires longer exposure times to be effective.
What type of sterilization is currently used in dentistry?
The most widely used sterilization method in dentistry is autoclaving (steam sterilization). It is preferred because it is highly effective in killing all forms of microbial life, including spores, and works quickly compared to other methods.
Other methods used in dentistry include:
- Dry heat sterilization (for heat-resistant instruments).
- Chemical sterilization (for instruments that cannot withstand high heat).
- Ultrasonic cleaning (used before sterilization to remove debris from instruments).
What are the four methods of sterilization?
The four primary methods of sterilization include:
Autoclaving (Steam Sterilization):
- Uses moist heat and high pressure to kill microorganisms quickly.
- Common in hospitals, dental clinics, and laboratories.
Dry Heat Sterilization:
- Uses prolonged exposure to high temperatures without moisture.
- Suitable for instruments that cannot be sterilized with steam.
Chemical Sterilization:
- Uses gases or liquid disinfectants to kill microorganisms.
- Common for sterilizing delicate or heat-sensitive instruments.
Radiation Sterilization:
- Uses ionizing radiation (gamma rays or electron beams) to sterilize materials.
- Often used in manufacturing to sterilize disposable medical and dental products.
What is the process of dental sterilization?
Dental sterilization follows a systematic process to ensure patient safety and prevent infections. The main steps include:
1. Pre-cleaning:
- Instruments are first rinsed to remove visible debris.
- Ultrasonic cleaners or enzymatic solutions may be used to break down organic matter.
2. Disinfection:
- Instruments are submerged in a disinfectant solution to kill most microbes before sterilization.
3. Sterilization:
- Instruments are placed in an autoclave or other sterilization device.
- High-temperature steam, dry heat, or chemical agents destroy all microorganisms, including spores.
4. Storage:
- Sterilized instruments are sealed in sterile packaging until they are needed.
- Proper storage prevents recontamination before use.
Which kind of sterilization is most common in dental practice?
The most common sterilization method used in dental practices is autoclaving (steam sterilization). It is preferred because it:
- Provides rapid sterilization (15–30 minutes).
- Kills bacteria, viruses, fungi, and spores effectively.
- Is compatible with most metal dental instruments.
For materials that cannot withstand steam sterilization, alternative methods like dry heat, chemical sterilization, or gas sterilization may be used.
What is the most commonly used method of sterilization?
The autoclave (steam sterilization) is the most commonly used method in medical, dental, and laboratory settings because it is:
- Highly effective – Kills all microorganisms, including spores.
- Fast – Typically completes sterilization in 15–30 minutes.
- Safe for most instruments – Works well for metal tools and reusable instruments.
What are the new techniques of sterilization?
Recent advancements in sterilization technology include:
Hydrogen Peroxide Plasma Sterilization:
- Uses vaporized hydrogen peroxide and plasma to sterilize instruments.
- Faster than traditional gas sterilization and produces fewer toxic byproducts.
Ozone Sterilization:
- Uses ozone gas to eliminate microorganisms.
- A more environmentally friendly alternative to traditional gas sterilization.
UV Light Sterilization:
- Uses ultraviolet (UV-C) light to kill bacteria and viruses on surfaces and instruments.
- Often used as an additional method for surface sterilization in dental offices.
Supercritical Carbon Dioxide (SC-CO₂) Sterilization:
- A newer, eco-friendly method that uses supercritical CO₂ to sterilize heat-sensitive materials.
What is the difference between EtO and autoclave?
Ethylene Oxide (EtO) Sterilization:
- Uses ethylene oxide gas to sterilize instruments at low temperatures.
- Suitable for heat-sensitive materials like plastic and rubber.
- Requires a long aeration period to remove toxic residues.
Autoclave (Steam Sterilization):
- Uses high-pressure steam at temperatures of 121–134°C.
- Works quickly (15–30 minutes) and is widely used for metal instruments.
- Not suitable for heat-sensitive materials.
Key Differences:
- EtO sterilization is better for delicate instruments but takes longer and requires aeration.
- Autoclaving is faster and more common but limited to heat-resistant instruments.
How many minutes to autoclave?
Autoclave sterilization times depend on the temperature and type of instruments being sterilized:
- Unwrapped instruments: 15–30 minutes at 121°C (250°F).
- Wrapped instruments: 30–40 minutes at 121°C (250°F).
- Higher temperatures (132°C/270°F): Can reduce sterilization time to 3–10 minutes.
- Porous loads (e.g., cloth materials): 30–60 minutes at 121°C.
After sterilization, instruments need drying time to prevent contamination before use.
Conclusion
Sterilization is a cornerstone of infection control in dentistry, safeguarding the health of patients and dental professionals. By understanding and implementing effective sterilization techniques, dental practices can significantly reduce the risk of cross-contamination and ensure a safe clinical environment. Continuous education, adherence to protocols, and regular monitoring are essential to maintain high standards of sterilization and uphold the trust and safety of patients.