Multiple sclerosis (MS) is a chronic, potentially disabling disease of the central nervous system (CNS) that affects millions of people worldwide. It disrupts communication between the brain and the rest of the body, leading to a variety of physical and cognitive symptoms. This article provides an in-depth exploration of MS, including its causes, symptoms, diagnosis, treatment options, and ongoing research.
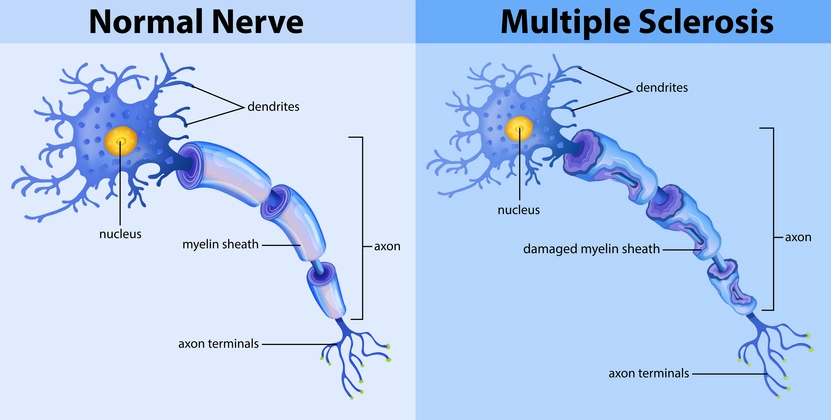
Table of Contents
ToggleWhat is Multiple Sclerosis?
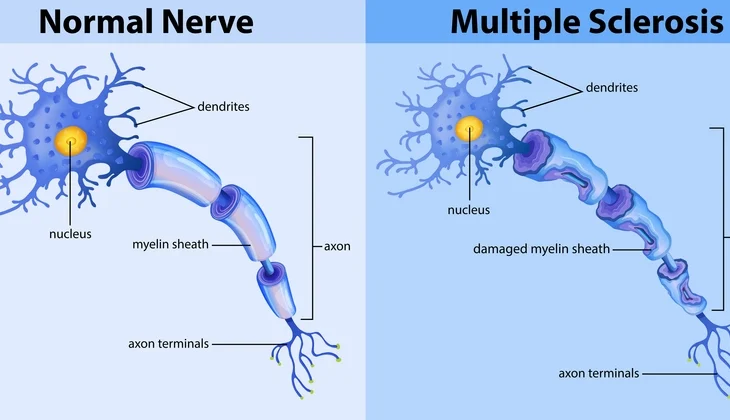
Multiple sclerosis is an autoimmune disease in which the body’s immune system mistakenly attacks the myelin sheath, the protective covering of nerve fibers in the CNS, which includes the brain and spinal cord. The damage results in inflammation and the formation of scar tissue (sclerosis), which disrupts the normal flow of electrical impulses along the nerves, leading to a wide range of symptoms. The severity of these symptoms depends on the extent of myelin damage and the specific nerves that are affected.
The CNS functions as the command center for the body, processing sensory information, controlling movement, and coordinating mental activities. The myelin sheath is essential for the rapid and efficient transmission of electrical signals between nerve cells. When the myelin is damaged, the signals slow down or become completely blocked, leading to neurological impairments.
MS is considered a heterogeneous disease, meaning that it presents differently in different individuals. Some people experience mild symptoms and long periods of remission, while others may face progressive worsening of their condition over time. The variability of MS makes it a particularly challenging disease to diagnose and manage. While it is not classified as a terminal illness, its impact on quality of life can be profound, affecting mobility, cognition, and overall well-being.
Additionally, MS is known as a “demyelinating disease,” which means that it specifically involves the destruction of myelin. Over time, repeated immune attacks can lead to permanent nerve damage and loss of function. Unlike some other neurological conditions, MS does not always follow a predictable course, and symptoms can fluctuate in intensity or suddenly worsen during what are known as “relapses” or “flare-ups.”
The disease is typically diagnosed in young adults, with the majority of cases emerging between the ages of 20 and 50. However, it can occur at any age, and women are affected more frequently than men. Due to its unpredictable nature, MS requires a multifaceted approach to treatment, focusing on symptom management, disease modification, and lifestyle adjustments to help individuals maintain a high quality of life.
Causes and Risk Factors
The exact cause of MS remains unknown, but it is believed to result from a combination of genetic, environmental, and lifestyle factors that contribute to immune system dysfunction. Researchers have identified several risk factors that may increase the likelihood of developing MS:
- Genetic Susceptibility
- Immune System Dysfunction
- Viral Infections
- Vitamin D Deficiency and Sunlight Exposure
- Smoking and Tobacco Use
- Geographic and Environmental Factors
- Gut Microbiome and Diet
- Obesity in Childhood and Adolescence
- Gender and Hormonal Influence
- Stress and Psychological Factors
Genetic Susceptibility
While MS is not directly inherited, genetic predisposition plays a role. People who have a close relative (such as a parent or sibling) with MS have a higher risk of developing the disease. Scientists have identified specific genetic variations associated with immune system regulation that may contribute to MS susceptibility.
Immune System Dysfunction
MS is classified as an autoimmune disease, meaning the immune system mistakenly attacks the body’s own tissues. In MS, the immune system targets myelin, leading to inflammation and nerve damage. The exact trigger for this immune response is still unclear, but it is thought to involve a combination of genetic predisposition and environmental factors.
Viral Infections
Certain viral infections have been linked to an increased risk of MS. The Epstein-Barr virus (EBV), which causes mononucleosis, is one of the strongest suspected triggers. Studies have shown that individuals who have had EBV infection are more likely to develop MS. Other viruses, such as human herpesvirus 6 (HHV-6) and cytomegalovirus (CMV), have also been investigated for their potential role in MS onset.
Vitamin D Deficiency and Sunlight Exposure
Vitamin D plays a crucial role in immune system function. People who have lower levels of vitamin D, often due to limited sun exposure, are at a higher risk of developing MS. This could explain why MS is more prevalent in regions farther from the equator, where sunlight exposure is lower.
Smoking and Tobacco Use
Smoking is a significant risk factor for MS. Studies have shown that smokers are more likely to develop MS compared to non-smokers. Additionally, smoking may accelerate disease progression and worsen symptoms in individuals who already have MS.
Geographic and Environmental Factors
MS is more common in temperate regions such as North America, Europe, and parts of Australia and New Zealand. The reason for this geographic distribution is not fully understood but is thought to be linked to environmental factors such as sunlight exposure, diet, and potential exposure to infectious agents.
Gut Microbiome and Diet
Emerging research suggests that the gut microbiome—the collection of bacteria and other microorganisms in the digestive tract—may influence immune system function and contribute to MS risk. Certain dietary patterns, including high-fat and high-sugar diets, have been linked to increased inflammation, which may play a role in the development of autoimmune diseases like MS.
Obesity in Childhood and Adolescence
There is growing evidence that obesity during childhood and adolescence may increase the risk of developing MS later in life. Excess body fat is associated with chronic inflammation and immune system dysfunction, which may contribute to the onset of MS in genetically susceptible individuals.
Gender and Hormonal Influence
MS is more common in women than in men, suggesting that hormonal differences may play a role in disease development. Estrogen and progesterone, which fluctuate during the menstrual cycle, pregnancy, and menopause, are believed to influence immune system activity. Some studies suggest that pregnancy may have a temporary protective effect against MS relapses, while others indicate that hormonal changes during menopause may exacerbate symptoms.
Stress and Psychological Factors
Chronic stress and psychological trauma have been investigated as potential risk factors for MS. While the link is not fully established, stress is known to affect immune system function, and some studies suggest that severe stress may trigger relapses or worsen symptoms in individuals already diagnosed with MS.
Types of Multiple Sclerosis
MS manifests in different forms, each with its unique progression and symptom severity. The main types of MS include:
- Relapsing-Remitting MS (RRMS)
- Primary Progressive MS (PPMS)
- Secondary Progressive MS (SPMS)
- Progressive-Relapsing MS (PRMS)
Relapsing-Remitting MS (RRMS)
The most common form, affecting approximately 85% of MS patients. It is characterized by periods of relapse, where symptoms worsen, followed by remission, where symptoms partially or completely recover. Over time, some individuals with RRMS may transition into secondary progressive MS.
Primary Progressive MS (PPMS)
A less common form, affecting about 10-15% of individuals with MS. PPMS is characterized by a steady progression of symptoms from the onset without distinct relapses or remissions. Patients with PPMS may experience gradual worsening of mobility and neurological function.
Secondary Progressive MS (SPMS)
This form develops in individuals who initially had RRMS. Over time, relapses become less frequent, but neurological function continues to decline progressively. SPMS can vary in severity, with some individuals experiencing a slow decline while others progress more rapidly.
Progressive-Relapsing MS (PRMS)
The rarest type of MS, marked by a steady worsening of symptoms with occasional acute relapses. Unlike RRMS, there are no periods of remission, and symptoms continuously worsen over time.
Symptoms of MS
The symptoms of MS vary widely among individuals and depend on the extent and location of nerve damage. Common symptoms include:
- Fatigue
- Numbness and Tingling
- Muscle Weakness and Spasms
- Vision Problems
- Balance and Coordination Issues
- Cognitive Impairment
- Bladder and Bowel Dysfunction
- Emotional and Mood Changes
Fatigue
A persistent sense of exhaustion that affects daily activities, even after rest. It is one of the most common and debilitating symptoms of MS.
Numbness and Tingling
Often experienced in the face, arms, legs, or trunk. These sensations can range from mild tingling to complete loss of sensation.
Muscle Weakness and Spasms
Can lead to difficulties with movement, coordination, and even walking. Muscle stiffness and painful spasms, known as spasticity, are also common.
Vision Problems
Blurred vision, double vision, and optic neuritis (inflammation of the optic nerve) can cause temporary or permanent vision loss in severe cases.
Balance and Coordination Issues
MS can affect the cerebellum, leading to dizziness, vertigo, and unsteady movements, increasing the risk of falls.
Cognitive Impairment
Difficulties with memory, concentration, and processing information, often referred to as “brain fog.”
Bladder and Bowel Dysfunction
Urinary urgency, incontinence, constipation, and bowel control issues are common in MS patients.
Emotional and Mood Changes
Depression, anxiety, and mood swings are frequent, often due to both neurological and psychological factors related to MS.
MS symptoms can vary in intensity and may come and go unpredictably, requiring tailored management strategies for each individual.
Diagnosis of Multiple Sclerosis
Diagnosing MS can be challenging due to its diverse symptoms, which often mimic those of other neurological conditions. There is no single test to confirm MS, so a comprehensive diagnostic process is required, incorporating medical history, neurological examinations, imaging, and laboratory tests.
Medical History and Physical Examination
A neurologist will conduct a thorough assessment, reviewing the patient’s medical history and symptoms. The physician will evaluate neurological function, checking for abnormalities in reflexes, balance, coordination, vision, and sensory responses.
Magnetic Resonance Imaging (MRI)
MRI is the most effective imaging technique for detecting MS. It uses powerful magnets and radio waves to create detailed images of the brain and spinal cord, helping to identify lesions or plaques caused by demyelination. Gadolinium contrast dye is often used to differentiate between old and new lesions, providing insight into disease activity and progression.
Lumbar Puncture (Spinal Tap)
A lumbar puncture involves collecting cerebrospinal fluid (CSF) from the lower spine to test for abnormalities associated with MS. The presence of oligoclonal bands (OCBs), which indicate an abnormal immune response in the CNS, supports an MS diagnosis. However, this test alone is not conclusive and is usually used alongside MRI findings.
Evoked Potential Tests
These tests measure the electrical activity of the brain in response to stimuli, such as visual, auditory, or sensory signals. Delays in the nerve signals can indicate MS-related nerve damage even before noticeable symptoms develop.
Blood Tests
Although no specific blood test can diagnose MS, they are used to rule out other conditions that mimic MS, such as lupus, Lyme disease, vitamin B12 deficiency, or neuromyelitis optica spectrum disorder (NMOSD).
The McDonald Criteria for MS Diagnosis
The McDonald criteria, developed by the International Panel on MS Diagnosis, help physicians diagnose MS with greater accuracy. The criteria require evidence of:
- Lesions in different areas of the CNS (dissemination in space)
- Lesions occurring at different times (dissemination in time)
- No other plausible explanation for the symptoms
If MS is strongly suspected but does not meet all criteria, patients may be diagnosed with “clinically isolated syndrome” (CIS) and monitored for further disease activity.
Differential Diagnosis
Because MS shares symptoms with other neurological and autoimmune diseases, physicians must rule out alternative explanations. Conditions such as stroke, migraines, fibromyalgia, and autoimmune diseases like sarcoidosis or Sjogren’s syndrome can present similar neurological symptoms.
Treatment Options for MS
Although there is no cure for MS, several treatment options help manage symptoms, slow disease progression, and improve quality of life. Treatment approaches typically fall into three main categories: disease-modifying therapies (DMTs), symptom management, and lifestyle modifications.
Disease-Modifying Therapies (DMTs)
DMTs help reduce the frequency and severity of relapses, slow the progression of disability, and minimize new lesions in the brain and spinal cord. These treatments are most effective in relapsing-remitting MS (RRMS) and some cases of secondary progressive MS (SPMS). Common DMTs include:
Injectable Therapies:
- Interferon beta medications (e.g., Avonex, Rebif, Betaseron) – reduce immune system activity and decrease inflammation.
- Glatiramer acetate (Copaxone) – mimics myelin proteins to divert immune attacks away from nerve fibers.
Oral Medications:
- Fingolimod (Gilenya) – prevents immune cells from reaching the CNS.
- Dimethyl fumarate (Tecfidera) – reduces inflammation and oxidative stress in nerve cells.
- Siponimod (Mayzent) – slows progression in secondary progressive MS.
- Cladribine (Mavenclad) – suppresses immune system activity.
Infusion Therapies:
- Natalizumab (Tysabri) – prevents immune cells from entering the brain and spinal cord.
- Ocrelizumab (Ocrevus) – targets B-cells, reducing immune system attacks.
- Alemtuzumab (Lemtrada) – depletes immune cells responsible for attacking myelin.
Each DMT has potential side effects, and the choice of therapy depends on disease severity, patient lifestyle, and response to treatment. Regular monitoring is necessary to assess effectiveness and manage side effects.
Symptomatic Treatments
Managing MS symptoms is essential for improving quality of life. Various medications and therapies address common MS-related issues, including:
- Fatigue: Amantadine, modafinil, and energy management strategies can help reduce fatigue.
- Muscle Spasms and Stiffness: Baclofen, tizanidine, and physical therapy help manage spasticity.
- Pain Management: Gabapentin, pregabalin, and acupuncture can relieve nerve pain.
- Bladder and Bowel Dysfunction: Anticholinergic medications help control bladder urgency, while dietary changes and laxatives address constipation.
- Cognitive Impairments: Cognitive rehabilitation therapy, memory training, and medications such as donepezil may assist with brain function.
- Depression and Anxiety: Antidepressants, therapy, and mindfulness practices help improve mental well-being.
Rehabilitation and Supportive Therapies
- Physical Therapy (PT): PT helps improve strength, balance, and mobility through tailored exercises and assistive devices like canes and braces.
- Occupational Therapy (OT): OT provides adaptive strategies to maintain independence in daily tasks such as dressing, cooking, and writing.
- Speech Therapy: Helps with communication difficulties and swallowing issues that arise due to MS-related muscle weakness.
- Cognitive Therapy: Assists in improving memory, problem-solving, and focus.
- Psychological Counseling and Support Groups: Emotional support and coping strategies help MS patients manage the mental and social impact of the disease.
Lifestyle Modifications and Holistic Approaches
While medications play a critical role, lifestyle changes significantly impact disease management and overall health:
- Regular Exercise: Low-impact activities like yoga, swimming, and stretching improve mobility, reduce spasticity, and enhance mood.
- Balanced Diet: A diet rich in omega-3 fatty acids, antioxidants, and whole foods may support brain health and reduce inflammation.
- Adequate Sleep: Proper rest is essential for managing fatigue and cognitive function.
- Stress Management: Meditation, mindfulness, and breathing exercises help lower stress levels, which can trigger MS relapses.
- Smoking Cessation and Alcohol Moderation: Avoiding smoking and limiting alcohol intake can help slow disease progression.
Experimental and Emerging Treatments
Ongoing research is focused on discovering new treatments and potential cures for MS. Some promising approaches include:
- Stem Cell Therapy (HSCT): Hematopoietic stem cell transplantation (HSCT) is an experimental therapy that aims to reset the immune system and halt MS progression.
- Remyelination Therapies: Scientists are studying ways to repair myelin damage and restore nerve function.
- Neuroprotective Drugs: Research is exploring medications that protect nerve cells from degeneration.
- Gut Microbiome Research: Investigating how gut bacteria influence the immune system and contribute to MS.
Research and Future Directions
Despite significant advances in understanding and treating multiple sclerosis, ongoing research continues to explore new therapies and uncover the underlying mechanisms of the disease. Future MS research focuses on disease-modifying treatments, remyelination strategies, neuroprotection, and understanding environmental and genetic risk factors.
Advances in Disease-Modifying Therapies (DMTs)
New and improved DMTs are continuously being developed to provide more effective ways to manage MS while minimizing side effects. Current research includes:
- Next-generation monoclonal antibodies: More targeted therapies that reduce immune system attacks with fewer adverse effects.
- Personalized medicine: Using biomarkers and genetic profiles to tailor treatments to individual patients for better outcomes.
- Combination therapies: Exploring whether combining different DMTs can provide better disease control while reducing relapse rates.
Remyelination and Nerve Repair
One of the most promising areas of MS research is remyelination therapy—restoring the protective myelin sheath around nerves. Scientists are investigating ways to stimulate the body’s ability to regenerate myelin. Key approaches include:
- Stem cell therapy: Hematopoietic stem cell transplantation (HSCT) is being studied as a way to reset the immune system and encourage myelin repair.
- Oligodendrocyte activation: Oligodendrocytes are the cells responsible for producing myelin. Research is focusing on ways to promote their activity and encourage remyelination.
- Experimental drugs: Potential therapies, such as clemastine fumarate, are being tested for their ability to restore myelin and improve nerve function.
Neuroprotection Strategies
Since nerve damage is a major driver of MS progression, researchers are investigating ways to protect nerve cells from degeneration. Neuroprotective strategies include:
- Antioxidant therapies: Studying the role of oxidative stress in MS and how antioxidants can prevent nerve damage.
- Mitochondrial support: Investigating ways to improve mitochondrial function in nerve cells to reduce energy depletion and cell death.
- Inflammation control: Developing treatments to reduce chronic inflammation and slow disease progression.
Role of the Gut Microbiome
Recent research has shown that the gut microbiome—the collection of bacteria and other microorganisms in the digestive tract—may play a role in regulating immune function. Scientists are exploring:
- How gut bacteria influence immune system activity and MS risk.
- Probiotics and dietary interventions to modulate the gut microbiome for better MS management.
- Fecal microbiota transplantation (FMT) as a potential therapy for immune system regulation.
Genetic and Environmental Research
Understanding why some individuals develop MS while others do not is a major research focus. Studies aim to:
- Identify genetic markers that contribute to MS susceptibility.
- Determine how environmental factors, such as infections, vitamin D levels, and lifestyle habits, influence MS development.
- Analyze the role of Epstein-Barr virus (EBV) and other viruses in triggering MS.
Emerging Technologies in MS Research
Advancements in technology are revolutionizing how MS is studied and managed. Some promising developments include:
- Artificial intelligence (AI): Using AI and machine learning to analyze large datasets and predict disease progression.
- Wearable devices: Smart technology that tracks symptoms and mobility changes to provide real-time insights into disease progression.
- Advanced imaging techniques: Improved MRI technology is allowing researchers to visualize brain changes in more detail, helping with early diagnosis and treatment monitoring.
Potential Future Cures
While no cure for MS exists yet, several innovative therapies are being explored as potential long-term solutions:
- Gene therapy: Scientists are investigating gene-editing technologies like CRISPR to correct genetic mutations linked to MS.
- Immune system reprogramming: Strategies to reset the immune system and prevent it from attacking myelin in the first place.
- Regenerative medicine: Research into ways to completely restore damaged nerves and reverse MS symptoms.
Living with Multiple Sclerosis
A diagnosis of MS can be life-altering, but with the right support, treatment, and lifestyle adjustments, individuals can still lead fulfilling lives. Managing MS involves addressing both physical and emotional challenges while maintaining independence and a positive outlook. Here are key aspects of living with MS:
Managing Symptoms Effectively
Since MS symptoms vary widely, individualized treatment plans are essential. Common strategies include:
- Medication adherence: Consistently following prescribed treatments, including disease-modifying therapies (DMTs), can slow disease progression and reduce relapses.
- Physical therapy: Regular physical therapy sessions help improve strength, flexibility, and mobility while reducing muscle stiffness and spasticity.
- Pain management: Medications, acupuncture, and relaxation techniques can help alleviate MS-related pain.
- Energy conservation: Managing fatigue through planned rest breaks, prioritizing activities, and using mobility aids when necessary.
Adapting to Physical Limitations
Mobility challenges may arise as MS progresses, making accessibility modifications necessary:
- Assistive devices: Canes, walkers, wheelchairs, and braces help maintain mobility and independence.
- Home modifications: Installing ramps, grab bars, and stairlifts can enhance safety and ease of movement.
- Occupational therapy: Helps individuals adapt daily tasks to accommodate physical changes and maximize independence.
Emotional and Mental Health Support
MS can have a significant psychological impact, often leading to depression, anxiety, and cognitive difficulties. Coping strategies include:
- Counseling and therapy: Speaking with mental health professionals can provide emotional support and coping strategies.
- Support groups: Connecting with others living with MS fosters a sense of community and reduces feelings of isolation.
- Mindfulness and stress management: Techniques such as meditation, yoga, and deep breathing exercises can help improve mental well-being.
Maintaining an Active Lifestyle
Regular physical activity can enhance overall health and well-being. Recommended activities include:
- Low-impact exercise: Swimming, yoga, and stretching help improve flexibility and reduce stiffness.
- Strength training: Light resistance exercises can maintain muscle strength and function.
- Aerobic activities: Walking and cycling (if feasible) promote cardiovascular health.
- Listening to the body: Adjusting activity levels based on fatigue and energy levels is essential.
Nutrition and Diet
A well-balanced diet plays a crucial role in managing MS symptoms and overall health:
- Anti-inflammatory foods: Consuming foods rich in omega-3 fatty acids (salmon, flaxseeds) and antioxidants (fruits and vegetables) can help reduce inflammation.
- Hydration: Staying hydrated supports cognitive function and reduces fatigue.
- Vitamin D and calcium: Important for bone health, especially in individuals with limited mobility.
- Avoiding processed foods and excess sugar: Helps regulate energy levels and supports overall well-being.
Navigating Work and Social Life
Living with MS may require adjustments in the workplace and social settings:
- Workplace accommodations: Flexible schedules, remote work options, and ergonomic workstations can help manage symptoms while remaining productive.
- Communicating with employers: Disclosing an MS diagnosis to employers (if comfortable) may lead to accommodations under disability laws.
- Maintaining social connections: Staying engaged with friends, family, and hobbies is essential for emotional well-being.
Planning for the Future
Long-term planning can provide peace of mind and financial security:
- Disability benefits: Understanding disability rights and eligibility for financial support programs can be helpful.
- Advance care planning: Discussing long-term healthcare preferences with loved ones ensures proper care decisions in the future.
- Legal considerations: Setting up a power of attorney and living will can ensure decisions align with personal wishes.
Frequently Asked Questions (FAQs)
Can people live a normal life with MS?
Yes, many people with MS can lead fulfilling lives with proper management and treatment. With advancements in medication, rehabilitation therapies, and lifestyle modifications, individuals can maintain their independence, work, and engage in social activities. Emotional support and a strong healthcare team play a significant role in helping people with MS live a high-quality life.
What is multiple sclerosis caused by?
MS is an autoimmune disease in which the immune system mistakenly attacks the myelin sheath, the protective covering of nerves in the central nervous system. The exact cause remains unknown, but researchers believe a combination of genetic predisposition and environmental factors—such as viral infections, low vitamin D levels, and smoking—may contribute to the development of the disease.
Can MS patients marry?
Yes, people with MS can marry and have relationships like anyone else. While the condition may present challenges, such as fatigue or mobility issues, strong communication, understanding, and mutual support help individuals with MS build and maintain successful marriages and relationships. Many couples find ways to adapt and lead fulfilling lives together.
What happens to a person with multiple sclerosis?
MS affects the nervous system, leading to a wide range of symptoms that can vary from person to person. Common symptoms include fatigue, difficulty walking, numbness or tingling, muscle weakness, vision problems, balance and coordination issues, cognitive impairment, and bladder or bowel dysfunction. The severity and progression of MS differ for each individual, with some experiencing mild symptoms and others facing more significant challenges over time.
Can MS be cured?
There is currently no cure for MS, but various treatment options can help manage symptoms, reduce flare-ups, and slow the progression of the disease. Medications such as disease-modifying therapies (DMTs), physical therapy, lifestyle changes, and alternative therapies like acupuncture or meditation can improve quality of life. Ongoing research is focused on finding more effective treatments and, ultimately, a cure.
What age does MS start?
MS is most commonly diagnosed between ages 20 and 40, but it can occur at any age. Some cases have been reported in children (pediatric MS), while others are diagnosed later in life. Early detection and intervention can make a significant difference in disease management and long-term outcomes.
Can MS go away?
MS is a chronic condition, meaning it does not completely go away. However, some people experience periods of remission where symptoms improve or disappear for a time, particularly in the relapsing-remitting form of MS (RRMS). While these remissions can last months or even years, symptoms often return eventually. Long-term treatment and lifestyle adjustments can help manage the condition effectively.
Is MS painful?
Yes, MS can cause various types of pain, including nerve pain, muscle spasms, and musculoskeletal discomfort. Pain may be chronic or occur intermittently, depending on the type and severity of nerve damage. Management strategies include medications, physical therapy, stretching exercises, and alternative treatments such as massage and acupuncture.
Can stress cause MS?
Stress does not directly cause MS, but it may play a role in exacerbating symptoms and triggering relapses. Managing stress through relaxation techniques, mindfulness, counseling, and a healthy lifestyle can help improve overall well-being and reduce the impact of MS-related symptoms.
Can MS be stopped if caught early?
While MS cannot be completely stopped, early diagnosis and treatment can significantly slow its progression and reduce the frequency and severity of relapses. Disease modifying therapies (DMTs), lifestyle changes, and symptom management strategies can help people with MS maintain function and quality of life for a longer period.
Who is at high risk for MS?
Several factors increase the risk of developing MS, including genetics (having a family member with MS), environmental influences (low vitamin D levels, lack of sunlight exposure), infections (such as Epstein-Barr virus), smoking, and being female (women are more likely to develop MS than men). MS is also more common in certain geographical regions with higher latitudes.
Is MS genetic?
While MS is not directly inherited, having a close family member with MS increases the risk. Researchers believe that a combination of genetic susceptibility and environmental triggers leads to the development of MS. However, most people with a family history do not develop the disease, indicating that other factors are also at play.