Orthodontics is a specialized field of dentistry focused on diagnosing, preventing, and treating malocclusions or misalignments of teeth and jaws. A core aspect of orthodontic treatment is achieving desired tooth movement, which involves applying controlled mechanical forces to teeth. This article delves into the biological and mechanical principles behind tooth movement in orthodontics, providing an in-depth understanding of the process.
Table of Contents
ToggleIntroduction to Orthodontic Tooth Movement
Orthodontic tooth movement (OTM) is a biological process that occurs in response to external forces applied through appliances such as braces, clear aligners, or other devices. The movement relies on a well-coordinated response from periodontal tissues, including the periodontal ligament (PDL), alveolar bone, and surrounding structures.
Tooth movement is essential for correcting dental malocclusions, improving oral function, and enhancing aesthetics. The underlying mechanisms are complex and involve a combination of biomechanical forces and cellular responses.
Biomechanics of Tooth Movement
Orthodontic tooth movement occurs when a force is applied to a tooth, resulting in pressure and tension in the periodontal ligament. This process can be divided into three main phases:
- Initial Phase
- Lag Phase
- Post-Lag or Progressive Phase
Initial Phase
When an orthodontic force is applied, the tooth moves within its socket almost immediately. This movement is minimal and occurs due to the displacement of fluid within the PDL and compression of the surrounding tissues. This phase is temporary and lasts for approximately 1-2 days.
Lag Phase
The lag phase, lasting weeks, is characterized by a pause in noticeable tooth movement. During this time, hyalinization (cell death) occurs in the compressed PDL, necessitating the recruitment of osteoclasts to remove the necrotic tissue. Bone remodeling begins during this phase.
Post-Lag or Progressive Phase
After the lag phase, consistent tooth movement resumes. Bone resorption and deposition occur in response to the applied force, allowing the tooth to move within its socket. This phase continues as long as the force remains effective and appropriately applied.
Biological Basis of Tooth Movement
The biological mechanism of orthodontic tooth movement hinges on the dynamic interplay between mechanical forces, cellular activities, and biochemical signaling pathways. The following are the key components involved in the process:
- Periodontal Ligament (PDL)
- Alveolar Bone Remodeling
- Cellular Response
- Biochemical Mediators
Periodontal Ligament (PDL)
The PDL is a fibrous connective tissue that anchors the tooth to the alveolar bone. It plays a crucial role in sensing and transmitting forces applied to the tooth. The PDL contains cells such as fibroblasts, cementoblasts, and osteoblasts, along with extracellular matrix components like collagen fibers and proteoglycans.
When a force is applied, the PDL experiences areas of tension and compression:
- Tension: Fibroblasts in the PDL produce collagen fibers to facilitate bone deposition.
- Compression: The compressed PDL stimulates osteoclast activity, leading to bone resorption.
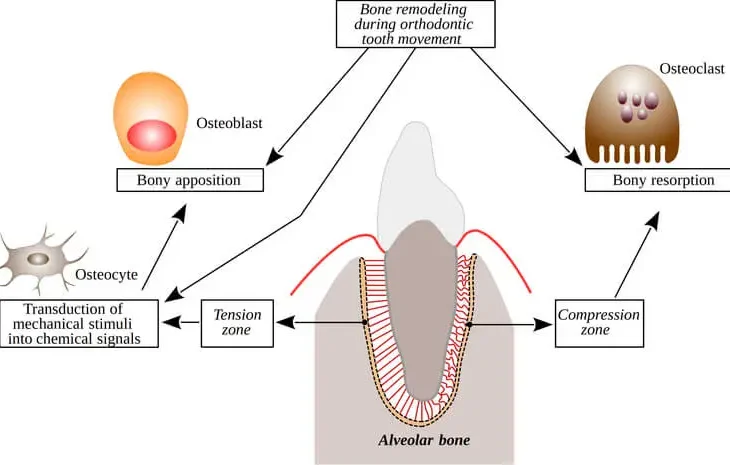
Alveolar Bone Remodeling
Bone remodeling is fundamental to tooth movement. It involves two key processes:
- Bone Resorption: Osteoclasts, specialized cells derived from monocytes, break down bone on the pressure side of the tooth.
- Bone Deposition: Osteoblasts, derived from mesenchymal stem cells, form new bone on the tension side.
The coupling of resorption and deposition ensures the tooth moves within its socket while maintaining structural integrity.
Cellular Response
Orthodontic forces activate various cell types, including:
- Osteoclasts: Responsible for bone resorption.
- Osteoblasts: Facilitate bone formation.
- Fibroblasts: Contribute to the remodeling of the PDL.
- Immune Cells: Such as macrophages, which play a role in inflammation and tissue repair.
Biochemical Mediators
Cellular response to orthodontic forces is mediated by biochemical signals, including:
- Cytokines: Such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α).
- Prostaglandins: Involved in bone remodeling and inflammatory responses.
- RANK/RANKL/OPG Pathway: Regulates osteoclast differentiation and activity.
- Nitric Oxide (NO): Facilitates cellular signaling during remodeling.
These mediators orchestrate the recruitment and activation of cells necessary for bone remodeling.
Types of Orthodontic Forces
The type, magnitude, and duration of force play critical roles in determining the efficacy and safety of tooth movement. Orthodontic forces can be categorized as:
1. Continuous Forces
Continuous forces are applied steadily over time, such as those from fixed braces. These forces maintain a consistent level of pressure on the tooth.
2. Intermittent Forces
Intermittent forces are applied periodically, as seen with removable appliances like clear aligners. The force is reactivated each time the appliance is worn.
3. Light vs. Heavy Forces
- Light Forces: These allow gradual and controlled tooth movement with minimal tissue damage and discomfort.
- Heavy Forces: Excessive forces can lead to hyalinization, delayed tooth movement, and potential root resorption.
Factors Influencing Tooth Movement
Several factors affect the rate and quality of orthodontic tooth movement:
- Patient-Specific Factors
- Force Magnitude and Direction
- Duration of Force Application
Patient-Specific Factors
- Age: Younger individuals tend to have faster tooth movement due to higher cellular activity and bone turnover rates.
- Systemic Health: Conditions like osteoporosis or diabetes can impact bone remodeling.
- Medications: Drugs such as bisphosphonates, corticosteroids, and NSAIDs influence bone metabolism.
Force Magnitude and Direction
- Optimal force magnitude is essential to ensure efficient movement without damaging tissues.
- The direction of force determines the type of tooth movement (e.g., tipping, bodily movement, or rotation).
Duration of Force Application
- Prolonged application of force is required for sustained tooth movement.
- Periodic adjustments ensure consistent pressure on the teeth.
Potential Complications
While orthodontic treatment is generally safe, certain complications can arise:
- Root Resorption
- Pain and Discomfort
- Relapse
Root Resorption
Excessive or prolonged forces can cause the loss of root structure, known as root resorption. Regular monitoring via radiographs is crucial to detect and manage this condition.
Pain and Discomfort
Patients often experience transient pain due to pressure on the PDL and associated inflammation. This can be managed with over-the-counter analgesics.
Relapse
After orthodontic treatment, teeth may shift back to their original positions. Retainers are essential to maintain the results.
Advances in Orthodontic Tooth Movement
Modern advancements aim to improve the efficiency and comfort of orthodontic treatment. Some innovations include:
Clear Aligners
Clear aligners provide a discreet and comfortable alternative to traditional braces. They use controlled and sequential forces to achieve tooth movement.
Temporary Anchorage Devices (TADs)
TADs are small implants placed in the bone to provide stable anchorage for complex tooth movements.
Accelerated Orthodontics
Techniques like micro osteoperforations and vibration devices stimulate bone remodeling, reducing treatment time.
3D Imaging and Digital Workflow
Advanced imaging technologies and digital tools enable precise treatment planning and visualization of tooth movement.
Frequently Asked Questions (FAQs)
1. How long does orthodontic tooth movement take?
The duration varies depending on the complexity of the case, patient age, and biological response. Generally, orthodontic treatment lasts between 12 to 36 months.
2. Does orthodontic tooth movement hurt?
Patients often experience mild discomfort for a few days after appliance adjustments, but this typically subsides. Over-the-counter pain relievers can help manage any discomfort.
3. Can orthodontic treatment damage teeth?
When conducted properly, orthodontic treatment is safe. However, excessive forces or poor oral hygiene during treatment can lead to complications such as root resorption or enamel demineralization.
4. What happens if I don’t wear my retainer after treatment?
Failure to wear retainers can result in relapse, where teeth shift back to their original positions. Retainers help maintain the corrected alignment.
5. Is tooth movement faster with clear aligners or braces?
The speed of tooth movement depends on various factors, including compliance, treatment planning, and biological response. In some cases, clear aligners may be faster for minor corrections, but braces are often more effective for complex movements.
6. Are there ways to speed up orthodontic tooth movement?
Yes, techniques like micro-osteoperforations, vibration devices, and low-level laser therapy may accelerate the process. However, these should only be performed under professional supervision.
Conclusion
Orthodontic tooth movement is a meticulously orchestrated process that combines mechanical forces with biological responses. Understanding the underlying mechanisms is crucial for achieving safe and effective outcomes. Ongoing research and technological innovations continue to enhance the field, offering patients more efficient, comfortable, and predictable treatments. By appreciating the complexities of tooth movement, orthodontists can deliver optimal care tailored to each patient’s unique needs.