Carpal Tunnel Syndrome (CTS) is a medical condition resulting from the compression of the median nerve as it travels through the carpal tunnel in the wrist. It is a prevalent disorder, particularly among individuals who engage in repetitive hand and wrist movements, such as dentists. Dentists are at an increased risk for CTS due to the precise and sustained motions required during dental procedures. This article explores the relationship between dentistry and carpal tunnel syndrome, examining its causes, symptoms, risk factors, prevention strategies, and treatment options, particularly for dental professionals.
Table of Contents
ToggleUnderstanding Carpal Tunnel Syndrome
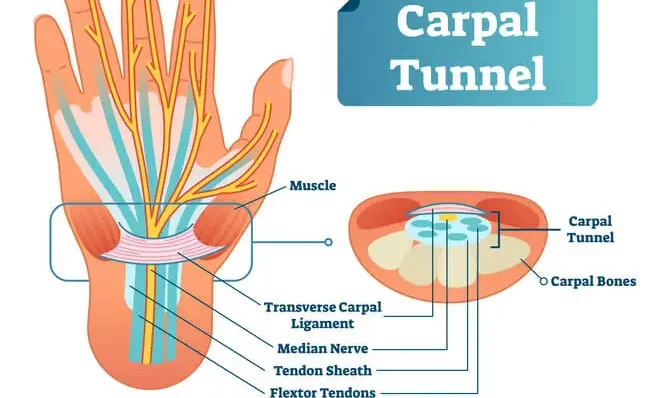
The carpal tunnel is a narrow passageway located on the palm side of the wrist. This tunnel houses several tendons and the median nerve, which is responsible for providing sensation to the thumb, index finger, middle finger, and part of the ring finger, as well as controlling some of the small muscles in the thumb. CTS occurs when this median nerve is compressed or irritated, leading to a variety of symptoms, including:
- Tingling or numbness
- Weakness
- Pain
Tingling or numbness
Patients often report these sensations in the thumb, index, and middle fingers. This may worsen at night or during activities involving wrist flexion.
Weakness
Affected individuals may experience weakness in the hand, making it difficult to perform tasks requiring grip strength.
Pain
Pain in the hand and wrist is common, sometimes extending up the arm toward the shoulder.
The progression of CTS can be gradual, starting with mild symptoms that increase in severity over time. If left untreated, it can lead to permanent nerve damage, resulting in muscle atrophy and significant hand dysfunction.
Prevalence of Carpal Tunnel Syndrome in Dentists
Dentists, dental hygienists, and other dental professionals are among the occupational groups most at risk for developing carpal tunnel syndrome. This is primarily due to the nature of their work, which involves intricate and repetitive movements of the hands and wrists. According to studies, the prevalence of CTS among dentists is higher than in many other healthcare professionals and workers in general.
Reasons for High Prevalence in Dental Professionals
- Repetitive hand and wrist movements
- Static postures
- Use of vibrating tools
- Work environment ergonomics
Repetitive hand and wrist movements
During dental procedures, dentists use tools in repetitive, small-scale movements that place continuous stress on the hand and wrist muscles and tendons. Over time, this can lead to inflammation and the compression of the median nerve.
Static postures
Dentists often hold static postures for prolonged periods while performing procedures, which further increases the strain on their hands, wrists, and arms. Sustained positions, especially those involving wrist flexion or extension, contribute to increased pressure in the carpal tunnel.
Use of vibrating tools
Many dental procedures require the use of high-speed, vibrating tools, such as drills. The vibrations from these instruments can irritate the tissues surrounding the median nerve, exacerbating the risk of CTS.
Work environment ergonomics
Poor ergonomic setup in dental offices, such as improperly adjusted chairs or inadequate lighting, can lead to unnatural wrist positions. These awkward postures put additional stress on the carpal tunnel.
Symptoms of Carpal Tunnel Syndrome in Dentists
The symptoms of CTS in dentists are similar to those experienced by the general population but may manifest more acutely due to the nature of their work. Common symptoms include:
- Numbness or tingling
- Pain
- Loss of dexterity
- Grip weakness
- Worsening symptoms at night
Numbness or tingling
Dentists may experience numbness or tingling in their fingers, particularly while gripping instruments during procedures.
Pain
Pain can develop not only in the hand and wrist but may also radiate up the forearm and into the shoulder.
Loss of dexterity
Dentists rely heavily on fine motor skills, and CTS can result in difficulty manipulating dental tools with precision.
Grip weakness
Reduced grip strength can make it challenging to hold and operate tools, compromising the quality of care provided to patients.
Worsening symptoms at night
Dentists often report that symptoms intensify during the night, possibly due to wrist flexion during sleep.
The impact of these symptoms on a dentist’s ability to perform their job effectively can be significant, leading to frustration, reduced productivity, and, in severe cases, career-ending impairments.
Risk Factors for Carpal Tunnel Syndrome in Dentists
Several factors increase the risk of developing CTS among dental professionals:
- Years of practice
- Gender
- Underlying medical conditions
- Pregnancy
- Genetic predisposition
Years of practice
The longer a dentist has been practicing, the greater the accumulated strain on their hands and wrists. CTS often develops after many years of continuous practice.
Gender
Women are more likely to develop CTS than men, potentially due to anatomical differences, such as having a narrower carpal tunnel.
Underlying medical conditions
Conditions like diabetes, arthritis, and hypothyroidism are associated with an increased risk of developing CTS. These conditions can contribute to inflammation and nerve compression.
Pregnancy
Pregnant women are at higher risk of developing CTS due to fluid retention, which can cause swelling in the wrist and increased pressure on the median nerve.
Genetic predisposition
Some individuals may have a genetic predisposition to developing CTS due to the size and shape of their carpal tunnel.
Prevention of Carpal Tunnel Syndrome in Dentists
Given the potential impact of CTS on a dentist’s career, prevention is crucial. While it may not always be possible to completely avoid CTS, several strategies can help reduce the risk of developing this condition:
- Ergonomic interventions
- Hand and wrist exercises
- Frequent breaks
- Work schedule management
- Maintaining overall health
Ergonomic interventions
- Proper chair and equipment positioning
- Proper lighting
- Tool design
Proper chair and equipment positioning
Dentists should ensure that their chairs and equipment are ergonomically positioned to allow for neutral wrist postures. Avoiding wrist flexion or extension during procedures can significantly reduce pressure on the median nerve.
Proper lighting
Adequate lighting can minimize the need for awkward postures, helping to reduce strain on the hands and wrists.
Tool design
Using tools with ergonomically designed handles that reduce the need for excessive force can also decrease wrist strain.
Hand and wrist exercises
Regular stretching and strengthening exercises for the hands, wrists, and forearms can improve flexibility and reduce the risk of injury. Exercises such as wrist flexor and extensor stretches, as well as nerve glides, are particularly helpful.
Performing these exercises during breaks or between procedures can help relieve accumulated tension in the wrists.
Frequent breaks
Dentists should schedule regular breaks throughout the workday to allow the hands and wrists to rest. Even short breaks can make a significant difference in reducing the cumulative strain on the carpal tunnel.
Work schedule management
Rotating tasks and avoiding prolonged periods of repetitive procedures can help distribute the physical load more evenly, minimizing the risk of CTS.
Maintaining overall health
Managing underlying health conditions such as diabetes and arthritis can reduce inflammation and improve overall nerve function, lowering the risk of CTS.
Staying physically active, maintaining a healthy weight, and practicing good posture outside of work also contribute to reducing the risk of developing CTS.
Treatment Options for Dentists with Carpal Tunnel Syndrome
For dentists who develop CTS, early diagnosis and intervention are critical to prevent permanent nerve damage. Treatment options range from conservative measures to surgical interventions, depending on the severity of the condition.
Non-surgical treatments
- Rest and activity modification
- Splinting
- Physical therapy
- Medications
Rest and activity modification
One of the first steps in treating CTS is to modify activities that exacerbate symptoms. Reducing repetitive hand movements and taking more frequent breaks can help reduce pressure on the median nerve.
Splinting
Wearing a wrist splint, particularly at night, can keep the wrist in a neutral position, reducing pressure on the median nerve. Splinting is often recommended for mild to moderate CTS cases.
Physical therapy
A physical therapist can develop a personalized exercise program to stretch and strengthen the muscles around the carpal tunnel, helping to alleviate symptoms and improve wrist function.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce inflammation and provide relief from pain. In some cases, corticosteroid injections may be used to reduce inflammation directly in the carpal tunnel.
Surgical treatments
For dentists with severe or persistent CTS that does not respond to conservative treatment, surgery may be necessary. Carpal tunnel release surgery is the most common surgical procedure used to treat CTS. This surgery involves cutting the ligament that forms the roof of the carpal tunnel to reduce pressure on the median nerve. There are two primary types of carpal tunnel release surgery:
- Open release surgery
- Endoscopic release surgery
Open release surgery
This traditional method involves making a small incision in the palm to access and release the carpal tunnel ligament.
Endoscopic release surgery
This minimally invasive technique involves using a small camera (endoscope) to guide the surgeon in cutting the ligament through smaller incisions. Recovery time for endoscopic surgery is typically shorter compared to open release surgery.
Frequently Asked Questions (FAQs)
Is carpal tunnel syndrome common in dentists?
Yes, carpal tunnel syndrome (CTS) is relatively common among dentists due to the repetitive hand and wrist movements required for dental procedures. Prolonged gripping of instruments and awkward wrist positions increase the risk.
How to prevent carpal tunnel syndrome for dentists?
Dentists can prevent CTS by:
- Using ergonomic tools and proper hand positioning
- Taking regular breaks and stretching hands and wrists
- Strengthening wrist and forearm muscles
- Wearing wrist supports or braces
- Maintaining proper posture during procedures
What jobs are most likely to get carpal tunnel?
Jobs that involve repetitive hand and wrist movements or prolonged gripping increase the risk of CTS. These include:
- Dentists and dental hygienists
- Assembly line workers
- Office workers (excessive typing and mouse use)
- Musicians
- Mechanics
- Cashiers and retail workers
How many dentists get carpal tunnel?
Studies suggest that a significant percentage of dentists, ranging from 15-35%, experience symptoms of CTS at some point in their careers due to the repetitive nature of their work.
What is commonly misdiagnosed as carpal tunnel?
Several conditions can mimic carpal tunnel syndrome, including:
- Cervical radiculopathy (pinched nerve in the neck)
- Thoracic outlet syndrome
- Arthritis
- Tendinitis
- Peripheral neuropathy
- Ganglion cysts
What are the red flags of carpal tunnel syndrome?
- Numbness or tingling in the thumb, index, and middle fingers
- Hand weakness, especially when gripping objects
- Pain that worsens at night
- Loss of fine motor skills
- Burning sensation in the wrist and fingers
What are the 5 stages of carpal tunnel?
- Mild: Occasional tingling, especially at night
- Moderate: Frequent numbness and pain during daily activities
- Severe: Constant pain, difficulty gripping objects
- Muscle Atrophy: Weakness and noticeable muscle wasting in the hand
- Permanent Damage: Irreversible nerve damage if untreated
What feels like carpal tunnel but isn’t?
Several conditions mimic CTS, such as:
- Cubital tunnel syndrome (affecting the ulnar nerve)
- De Quervain’s tenosynovitis
- Trigger finger
- Arthritis in the wrist or hand
- Pronator teres syndrome
Conclusion
Carpal tunnel syndrome is a common and potentially career-limiting condition for dentists, primarily due to the repetitive hand and wrist movements required in their profession. Recognizing the early symptoms of CTS and implementing preventative measures, such as ergonomic adjustments, regular breaks, and wrist exercises, can help reduce the risk of developing this condition. For dentists who do develop CTS, early intervention and treatment are critical to preserving hand function and preventing long-term damage. Whether through conservative measures or surgical intervention, effective treatment can allow dental professionals to continue practicing with reduced pain and improved hand function. Ultimately, raising awareness about the risks of CTS in dentistry and encouraging proactive prevention strategies is essential for safeguarding the health and longevity of dental professionals’ careers.